New Research
Updated July 21, 2021
Brain
Research paper of the month.
In this study from Iran, examining children in three different areas of the country with different levels of pollution, children living in the most polluted areas had IQs that were more than 16 points lower than children with the lowest amount of pollution.
Seifi M, Yunesian M, Naddafi K, Nabizadeh R, Dobaradaran S, Ziyarati MT, Nazmara S, Yekaninejad MS, Mahvi AH. Exposure to ambient air pollution and socio-economic status on intelligence quotient among schoolchildren in a developing country. Environ Sci Pollut Res Int. 2021 Aug 6. doi: 10.1007/s11356-021-15827-w. Epub ahead of print. PMID: 34355328.
Just 1 ug/m3 increase in PM2.5 corresponded to a 16% increase chance of Alzheimer’s
Shaffer R, et al. Fine Particulate Matter and Dementia Incidence in the Adult Changes in Thought Study. Environmental Health Perspectives, 2021; 129 (8): 087001 DOI: 10.1289/EHP9018
Indoor PM2.5 levels in offices associated with impaired cognition, attention span, response time, and productivity.
Jose Guillermo Cedeño Laurent, Piers MacNaughton, Emily
Jones, Anna S Young, Maya Bliss, Skye Flanigan, Jose Vallarino, Ling Jyh Chen, Xiaodong Cao, Joseph G Allen. Associations between acute exposures to PM2.5 and carbon dioxide indoors and cognitive function in office workers: a multicountry longitudinal prospective observational study. Environmental Research Letters, 2021; 16 (9): 094047 DOI: 10.1088/1748-9326/ac1bd8
Air pollution is associated with increased criminal behavior.
Herrnstadt, Evan, Anthony Heyes, Erich Muehlegger, and Soodeh Saberian. 2021. “Air Pollution and Criminal Activity: Microgeographic Evidence from Chicago.” American Economic Journal: Applied Economics, 13 (4): 70-100. DOI: 10.1257/app.20190091
Vigorous physical activity in air pollution increases brain white matter hyperintensity lesions, and air pollution attenuates the beneficial associations of physical activity with these lesions.
Melissa A. Furlong, Gene E. Alexander, Yann C. Klimentidis, David A. Raichlen. Association of Air Pollution and Physical Activity With Brain Volumes. Neurology, 2021; 10.1212/WNL.0000000000013031 DOI: 10.1212/WNL.0000000000013031
Reducing air pollution reduces the risk of dementia in older women.
Wang X, et al. Association of improved air quality with lower dementia risk in older women Proceedings of the National Academy of Sciences Jan 2022, 119 (2) e2107833119; DOI: 10.1073/pnas.2107833119
Air pollution causes inflammation and cell death of the olfactory system.
Wei S, Xu T, Jiang T, Yin D. Chemosensory Dysfunction Induced by Environmental Pollutants and Its Potential As a Novel Neurotoxicological Indicator: A Review. Environ Sci Technol. 2021 Aug 17;55(16):10911-10922. doi: 10.1021/acs.est.1c02048. Epub 2021 Aug 6. PMID: 34355568.
Kim BY, Park JY, Cho KJ, Bae JH. Effects of Urban Particulate Matter on the Olfactory System in a Mouse Model. Am J Rhinol Allergy. 2021 Jul 8:19458924211026416. doi: 10.1177/19458924211026416. Epub ahead of print. PMID: 34236242.
Older adults living in areas with higher PM2.5 concentrations had worse cognitive function even after adjustment for community- and individual-level social and economic characteristics.
Ailshire J, Crimmins E. Fine particulate matter air pollution and cognitive function among older US adults Am J Epidemiol. 2014 Aug 15;180(4):359-66. doi: 10.1093/aje/kwu155. Epub 2014 Jun 24.
Proximity to sources of airborne lead reduces brain function of children.
Gatzke-Kopp LM, Warkentien S, Willoughby M, Fowler C, Folch DC, Blair C. Proximity to sources of airborne lead is associated with reductions in Children’s executive function in the first four years of life. Health Place. 2021 Feb 2;68:102517. doi: 10.1016/j.healthplace.2021.102517
More evidence that rates of Alzheimers Dementia, including rates of mortality and hospital admission risks for AD, correlate with air pollution exposure.
Rhew SH, Kravchenko J, Lyerly HK. Exposure to low-dose ambient fine particulate matter PM2.5 and Alzheimer’s disease, non-Alzheimer’s dementia, and Parkinson’s disease in North Carolina. PLoS One. 2021;16(7):e0253253. Published 2021 Jul 9. doi:10.1371/journal.pone.0253253
Another study showing accelerated cognitive decline in the elderly exposed to more air pollution.
Duchesne J, et al. Exposure to ambient air pollution and cognitive decline: Results of the prospective Three-City cohort study. Environ Int. 2022 Feb 3;161:107118. doi: 10.1016/j.envint.2022.107118
Improvement in air quality was associated with less cognitive decline in the elderly
Younan D, Wang X, Millstein J, Petkus AJ, Beavers DP, Espeland MA, Chui HC, Resnick SM, Gatz M, Kaufman JD, Wellenius GA, Whitsel EA, Manson JE, Rapp SR, Chen JC. Air quality improvement and cognitive decline in community-dwelling older women in the United States: A longitudinal cohort study. PLoS Med. 2022 Feb 3;19(2):e1003893. doi: 10.1371/journal.pmed.1003893. eCollection 2022 Feb. PMID: 35113870
Letellier N, et al. Air quality improvement and incident dementia: Effects of observed and hypothetical reductions in air pollutant using parametric g-computation. Alzheimers Dement. 2022 Feb 9. doi: 10.1002/alz.12606
Higher exposure of pregnant mothers to PAHs in the third trimester delays and impairs emotional and behavioral development in infants.
Liu R, DeSerisy M, Fox NA, Herbstman JB, Rauh VA, Beebe B, Margolis AE. Prenatal exposure to air pollution and maternal stress predict infant individual differences in reactivity and regulation and socioemotional development. J Child Psychol Psychiatry. 2022 Feb 17. doi: 10.1111/jcpp.13581
In this animal study, evidence of the neurotoxicity and inflammatory effects of air pollution was confirmed with prolonged exposure to diesel exhaust causing impaired memory and learning, and triggered depressive like responses.
Ehsanifar M, Yavari Z, Rafati M. Exposure to urban air pollution particulate matter: neurobehavioral alteration and hippocampal inflammation. Environ Sci Pollut Res Int. 2022 Mar 3. doi: 10.1007/s11356-022-19367-9
More evidence that air pollution exposure early in life increases the risk of neurodevelopment disorders, especially attention deficit disorders, overall intelligence, and executive functioning.
Castagna A, Mascheron E, Fustinon S, Montiross R. Air pollution and neurodevelopmental skills in preschool- and school-aged children: A systematic review. Neurosci Biobehav Rev. 2022 Mar 21:104623. doi: 10.1016/j.neubiorev.2022.104623
Indoor levels of PM2.5 and CO2 were inversely associated with cognitive function in a prospective, longitudinal study that included working age subjects from six different countries.
Laurent JGC, MacNaughton P, Jones E, Young AS, Bliss M, Flanigan S, Vallarino J, Chen LJ, Cao X, Allen JG. Associations between Acute Exposures to PM2.5 and Carbon Dioxide Indoors and Cognitive Function in Office Workers: A Multicountry Longitudinal Prospective Observational Study.Environ Res Lett. 2021 Sep;16(9):094047. doi: 10.1088/1748-9326/ac1bd8. Epub 2021 Sep 9
Carbon monoxide exposure increases the risk of seizures in epileptic patients.
Chen Z, et al. Ambient air pollution and epileptic seizures: a panel study in Australia. Epilepsia. 2022 Apr 8. doi: 10.1111/epi.17253
More evidence that air pollution is toxic to the brain and is associated with neurologic diseases like Alzheimer’s and Parkinson’s Disease.
Patten K, et al. The Effects of Chronic Exposure to Ambient Traffic-Related Air Pollution on Alzheimer’s Disease Phenotypes in Wildtype and Genetically Predisposed Male and Female Rats. Environmental Health Perspectives, 2021; 129 (5) DOI: 10.1289/EHP8905
Jo S, Kim Y, Park KW, et al. Association of NO2 and Other Air Pollution Exposures With the Risk of Parkinson Disease. JAMA Neurol. Published online May 17, 2021. doi:10.1001/jamaneurol.2021.1335
Another study showing that even short-term air pollution exposure is associated with impaired cognition.
Gao X, et al. Short-term air pollution, cognitive performance and nonsteroidal anti-inflammatory drug use in the Veterans Affairs Normative Aging Study. Nature Aging, 2021; DOI: 10.1038/s43587-021-00060-4
Two new studies showing that prenatal and childhood air pollution exposure has lasting consequences to adolescent and adult behavior and academic performance.
Reuben A, et al. Association Of Air Pollution Exposure in Childhood and Adolescence With Psychopathology at the Transition To Adulthood. JAMA Network Open, 2021 DOI: 10.1001/jamanetworkopen.2021.7508
Margolis A, et al. Prenatal exposure to air pollution is associated with childhood inhibitory control and adolescent academic achievement. Environmental Research, 2021; 111570 DOI: 10.1016/j.envres.2021.111570
Closer proximity to sources of lead pollution is associated with loss of cognitive abilities and executive functioning in young children.
Gatzke-Kopp LM, Warkentien S, Willoughby M, Fowler C, Folch DC, Blair C. Proximity to sources of airborne lead is associated with reductions in Children’s executive function in the first four years of life. Health Place. 2021 Mar;68:102517. doi: 10.1016/j.healthplace.2021.102517. Epub 2021 Feb 2. PMID: 33540187; PMCID: PMC7965333
Fetal Development
Babies born within 3 km of an oil and gas drilling site had a lower birth weight than babies in the same area born before the drilling took place.
Willis M, et al. Associations between Residential Proximity to Oil and Gas Drilling and Term Birth Weight and Small-for-Gestational-Age Infants in Texas: A Difference-in-Differences Analysis. Environmental Health Perspectives, 2021; 129 (7): 077002 DOI: 10.1289/EHP7678
Wildfire smoke is associated with increased risk of low birth weight. 1 ug/m3 increase associated with a 2.17 gram reduction in birth weight, and an increase risk of low birth weight of 3% and a 12% increased risk for very low birth weight.
Jiajianghui Li, Tianjia Guan, Qian Guo, Guannan Geng, Huiyu Wang, Fuyu Guo, Jiwei Li, Tao Xue. Exposure to landscape fire smoke reduced birthweight in low- and middle-income countries: findings from a siblings-matched case-control study. eLife, 2021; 10 DOI: 10.7554/eLife.69298
More evidence that air pollution increases the risk of preterm birth and miscarriage especially with exposure at the late stage of pregnancy.
Zhou W, et al. Association between Maternal Exposure to Ambient Air Pollution and the Risk of Preterm Birth: A Birth Cohort Study in Chongqing, China, 2015-2020. Int J Environ Res Public Health. 2022 Feb 15;19(4):2211. doi: 10.3390/ijerph19042211.
Yu Z, Zhang X, Zhang J, Feng Y, Zhang H, Wan Z, Xiao C, Zhang H, Wang Q, Huang C. Gestational exposure to ambient particulate matter and preterm birth: An updated systematic review and meta-analysis. Environ Res. 2022 May 3:113381. doi: 10.1016/j.envres.2022.113381. Epub ahead of print. PMID: 35523275.
Zhou W, Ming X, Chen Q, Liu X, Yin P. The acute effect and lag effect analysis between exposures to ambient air pollutants and spontaneous abortion: a case-crossover study in China, 2017-2019. Environ Sci Pollut Res Int. 2022 May 6. doi: 10.1007/s11356-022-20379-8. Epub ahead of print. PMID: 35522417.
More evidence that air pollution causes systemic inflammation during pregnancy.
Zhang B, et al. Ambient PM2.5 exposures and systemic inflammation in women with early pregnancy.Sci Total Environ. 2022 Mar 14:154564. doi: 10.1016/j.scitotenv.2022.154564
Increased prenatal household air pollution exposure is associated with shorter telomere length at birth. Shorter TL at birth is associated with higher infant blood pressure. Pollution exposure in utero can affect cardiovascular health later in life.
Kaali S, et al. Prenatal Household Air Pollution Exposure, Cord Blood Mononuclear Cell Telomere Length and Age Four Blood Pressure: Evidence from a Ghanaian Pregnancy Cohort. Toxics. 2021 Jul 14;9(7):169. doi: 10.3390/toxics9070169. PMID: 34357912; PMCID: PMC8309911.
Sulfer dioxide, one of the component parts of air pollution in our valley, has been found to be associated with neural tube defects during the first month after conception.
Zhang JY, Dai HX, Wu QJ, Li J, Huang YH, Chen ZJ, Li LL, Chen YL, Liu S, Jiang CZ. Maternal exposure to ambient levels of sulfur dioxide and risk of neural tube defects in 14 cities in Liaoning province, China: a population-based case-control study. J Expo Sci Environ Epidemiol. 2020 Oct 1. doi: 10.1038/s41370-020-00273-6. Online ahead of print. PMID: 33005007
Exposure to traffic related air pollution during pregnancy increases the levels of pro-inflammatory chemicals like cytokines in cord blood, suggesting an impairment of immune function later in life.
García-Serna AM, et al. NELA Study Group. Cytokine profiles in cord blood in relation to prenatal traffic-related air pollution: The NELA cohort. Pediatr Allergy Immunol. 2022 Feb;33(2):e13732. doi: 10.1111/pai.13732. PMID: 35212052
In a first ever study, the prenatal/preconception pollution exposure of fathers was associated with lower birth weights.
Payne-Sturges DC, Puett R, Cory-Slechta DA. Both parents matter: a national-scale analysis of parental race/ethnicity, disparities in prenatal PM2.5 exposures and related impacts on birth outcomes. Environ Health. 2022 May 6;21(1):47. doi: 10.1186/s12940-022-00856-w. PMID: 35513869.
Another study that shows prenatal exposure affects lung disease vulnerability and rates of childhood asthma.
Wright R, et al. Prenatal Ambient Ultrafine Particle Exposure and Childhood Asthma in the Northeastern United States. American Journal of Respiratory and Critical Care Medicine, 2021; DOI: 10.1164/rccm.202010-3743OC
This is one of the first studies that shows prenatal exposure to air pollution critically impairs the production of thyroid hormones. Irizar A, et al. Association between prenatal exposure to air pollutants and newborn thyroxine (T4) levels. Environmental Research, 2021; 197: 111132 DOI: 10.1016/j.envres.2021.111132
Heart
New information on how air pollution injures the cells that line the blood vessels.
Li X, Haberzettl P, Conklin DJ, Bhatnagar A, Rouchka EC, Zhang M, O’Toole TE. Exposure to Fine Particulate Matter Air Pollution Alters mRNA and miRNA Expression in Bone Marrow-Derived Endothelial Progenitor Cells from Mice. Genes (Basel). 2021 Jul 10;12(7):1058. doi: 10.3390/genes12071058. PMID: 34356074; PMCID: PMC8307414.
Particulate pollution an road traffic noise increases the risk of hospital visits for cardiac arrhythmias and heart failure.
WU Jun Hui, WU Yao, WANG Zi Jing, TIAN Yao Hua, WU Yi Qun, WU Tao, WANG Meng Ying, WANG Xiao Wen, WANG Jia Ting, HU Yong Hua. Ambient Particulate Matter Pollution and Hospital Visits for Cardiac Arrhythmia in Beijing, China[J]. Biomedical and Environmental Sciences, 2021, 34(7): 562-566. doi: 10.3967/bes2021.077
Lim Y_H, et al. Long‐Term Exposure to Air Pollution, Road Traffic Noise, and Heart Failure Incidence: The Danish Nurse Cohort. Journal of the American Heart Association, 2021; DOI: 10.1161/JAHA.121.021436
Hourly increases in traffic related air pollution is association with significantly increased risk for heart attacks and impaired heart function. This association was attenuated by high levels of “residential greenness.”
Zhu Y, et al. Short-term exposure to traffic-related air pollution and STEMI events: Insights into STEMI onset and related cardiac impairment. Sci Total Environ. 2022 Feb 28:154210. doi: 10.1016/j.scitotenv.2022.154210
Chen R, Jiang Y, Hu J, Chen H, Li H, Meng X, Ji JS, Gao Y, Wang W, Liu C, Fang W, Yan H, Chen J, Wang W, Xiang D, Su X, Yu B, Wang Y, Xu Y, Wang L, Li C, Chen Y, Bell ML, Cohen AJ, Ge J, Huo Y, Kan H. Hourly Air Pollutants and Acute Coronary Syndrome Onset In 1.29 Million Patients. Circulation. 2022 Apr 22. doi: 10.1161/CIRCULATIONAHA.121.057179. Epub ahead of print. PMID: 35450432.
Ozone and nitrogen oxide levels in an area with high rates of wood burning were associated with a decrease in the diameter of the microscopic blood vessels in the eye, as well as higher blood pressure in children who lived in an area of high exposure to wood smoke. This is a clear indicator of the adverse impact of air pollution (in this case wood smoke) on blood vessels, and it shows up as early as childhood.
Korsiak J, Perepeluk KL, Peterson NG, Kulka R, Weichenthal S. Air pollution and retinal vessel diameter and blood pressure in school-aged children in a region impacted by residential biomass burning. Sci Rep. 2021 Jun 17;11(1):12790. doi: 10.1038/s41598-021-92269-x. PMID: 34140605
Two more studies showing that air pollution’s impact of increasing blood pressure begins in childhood.
Huang M, et al. Effects of Ambient Air Pollution on Blood Pressure Among Children and Adolescents: A Systematic Review and Meta‐Analysis. Journal of the American Heart Association, 2021; DOI: 10.1161/JAHA.120.017734
Prunicki M, et al. Air pollution exposure is linked with methylation of immunoregulatory genes, altered immune cell profiles, and increased blood pressure in children. Scientific Reports, 2021; 11 (1) DOI: 10.1038/s41598-021-83577-3
More evidence that the cardiovascular disease from air pollution involves stimulating white blood cell activity and inflammation.
Abohashem S, et al. A leucopoietic-arterial axis underlying the link between ambient air pollution and cardiovascular disease in humans. European Heart Journal, 2021 DOI: 10.1093/eurheartj/ehaa982
Wearing face masks to reduce pollution inhalation reduces the cardiovascular effects of the pollution.
Jiang M, Meng X, Qi L, Hu X, Xu R, Yan M, Shi Y, Meng X, Li W, Xu Y, Chen S, Zhu T, Gong J. The health effects of wearing face masks on cardiopulmonary system of healthy young adults: A double-blinded, randomized crossover trial. Int J Hyg Environ Health. 2021 Jul 12;236:113806. doi: 10.1016/j.ijheh.2021.113806. Epub ahead of print. PMID: 34265631.
Endocrine System
The incidence of metabolic syndrome dramatically increased in elderly males with exposure to particulate air pollution.
Zang ST, Luan J, Li L, Wu QJ, Chang Q, Dai HX, Zhao YH. Air pollution and metabolic syndrome risk: Evidence from nine observational studies. Environ Res. 2021 Jul 12:111546. doi: 10.1016/j.envres.2021.111546. Epub ahead of print. PMID: 34265350.
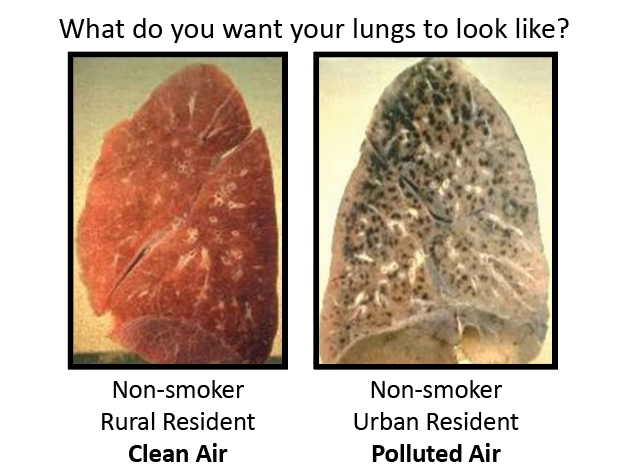
Lungs
New information on how air pollution harms the lungs, including inducing pulmonary fibrosis
Shim I, Kim W, Kim H, Lim YM, Shin H, Park KS, Yu SM, Kim YH, Sung HK, Eom IC, Kim P, Yu SD. Comparative Cytotoxicity Study of PM2.5 and TSP Collected
from Urban Areas. Toxics. 2021 Jul 14;9(7):167. doi: 10.3390/toxics9070167. PMID: 34357910; PMCID: PMC8309706.
Jia H, Liu Y, Guo D, He W, Zhao L, Xia S. PM2.5-induced pulmonary inflammation via activating of the NLRP3/caspase-1 signaling pathway. Environ Toxicol. 2020 Sep 30. doi: 10.1002/tox.23035.
Chang-Chien J, Huang JL, Tsai HJ, Wang SL, Kuo ML, Yao TC. Particulate matter causes telomere shortening and increase in cellular senescence markers in human lung epithelial cells. Ecotoxicol Environ Saf. 2021 Oct 1;222:112484. doi: 10.1016/j.ecoenv.2021.112484. Epub 2021 Jul 6. PMID: 34237641.
Geng Y, Cao Y, Zhao Q, Li Y, Tian S. Potential hazards associated with interactions between diesel exhaust particulate matter and pulmonary surfactant. Sci Total Environ. 2021 Oct 16:151031. doi: 10.1016/j.scitotenv.2021.151031
Shahabi R, et al. The effect of nanoparticles on pulmonary fibrosis: a systematic review and Meta-analysis of preclinical studies. Arch Environ Occup Health. 2022 Mar 4:1-11. doi: 10.1080/19338244.2021.2001637
Zhai X, Wang J, Sun J, Xin L. PM2.5 induces inflammatory responses via oxidative stress-mediated mitophagy in human bronchial epithelial cells. Toxicol Res (Camb). 2022 Jan 19;11(1):195-205. doi: 10.1093/toxres/tfac001. eCollection 2022 Feb. PMID: 35237424
Pollution is correlated with hospitalizations for bronchiectasis, especially in females and patients over 65 yrs. old.
Wang Z, et al. Association of hospital admission for bronchiectasis with air pollution: A province-wide time-series study in southern China. Int J Hyg Environ Health. 2020 Nov 3;231:113654. doi: 10.1016/j.ijheh.2020.113654.
More evidence that air pollution impairs lung function, and lung function growth in children.
Garcia E, Rice MB, Gold DR. Air pollution and lung function in children. J Allergy Clin Immunol. 2021 Jul;148(1):1-14. doi: 10.1016/j.jaci.2021.05.006. PMID: 34238501; PMCID: PMC8274324.
Lung function declines in children with asthma when exposed to multiple types of air pollution.
Kim Y, Park EH, Ng CFS, Chung Y, Hashimoto K, Tashiro K, Hasunuma H, Doi M, Tamura K, Moriuchi H, Nishiwaki Y, Kim H, Yi SM, Kim H, Hashizume M. Respiratory function declines in children with asthma associated with chemical species of fine particulate matter (PM2.5) in Nagasaki, Japan. Environ Health. 2021 Oct 21;20(1):110. doi: 10.1186/s12940-021-00796-x
Even short term pollution is harmful to lung function.
Renzi M, et al. A nationwide study of air pollution from particulate matter and daily hospitalizations for respiratory diseases in Italy. Sci Total Environ. 2021 Oct 16:151034. doi: 10.1016/j.scitotenv.2021.151034
Based on hospital admissions rates for respiratory diseases, this study concluded that wildfire PM2.5 is up to 10 times more harmful on human health than PM2.5 from other sources.
Aguilera, R., Corringham, T., Gershunov, A. et al. Wildfire smoke impacts respiratory health more than fine particles from other sources: observational evidence from Southern California. Nat Commun 12, 1493 (2021). https://doi.org/10.1038/s41467-021-21708-0
More evidence of particulate pollution exacerbating a person’s vulnerability to lung disease.
Wu Y, Jin T, He W, Liu L, Li H, Liu C, Zhou Y, Hong J, Cao L, Lu Y, Dong X, Xia M, Ding B, Qian L, Wang L, Zhou W, Gui Y, Zhang X, Chen R. Associations of fine particulate matter and constituents with pediatric emergency room visits for respiratory diseases in Shanghai, China. Int J Hyg Environ Health. 2021 Jul 13;236:113805. doi: 10.1016/j.ijheh.2021.113805. Epub ahead of print. PMID: 34271373.
Miscellaneous
Western wildfire smoke in 2020 was responsible for 19,000 cases of COVID and 700 deaths.
Xiaodan Zhou, Kevin Josey, Leila Kamareddine, Miah C. Caine, Tianjia Liu, Loretta J. Mickley, Matthew Cooper, Francesca Dominici. Excess of COVID-19 cases and deaths due to fine particulate matter exposure during the 2020 wildfires in the United
States. Science Advances, 2021; 7 (33): eabi8789 DOI: 10.1126/sciadv.abi8789
Each week of wildfire smoke exposures from fires in the state of Washington were estimated to cause 91 deaths, including 20 cardiovascular disease deaths, and 10 respiratory disease deaths. As climate change gets worse, the negative impacts of smoke will plague the Wasatch front more and more.
Liu Y, Austin E, Xiang J, Gould T, Larson T, Seto E. Health Impact Assessment of PM 2.5 attributable mortality from the September 2020 Washington State Wildfire Smoke Episode. medRxiv. 2020 Sep 22:2020.09.19.20197921. doi: 10.1101/2020.09.19.20197921
More evidence of the impact of air pollution on the risk of death from COVID
Bozack A, et al. Long-Term Air Pollution Exposure and COVID-19 Mortality: A Patient-Level Analysis from New York City. American Journal of Respiratory and Critical Care Medicine, 2021; DOI: 10.1164/rccm.202104-0845OC
Kogevinas M, et al. Ambient Air Pollution in Relation to SARS-CoV-2 Infection, Antibody Response, and COVID-19 Disease: A Cohort Study in Catalonia, Spain (COVICAT Study). Environmental Health Perspectives, 2021; 129 (11) DOI: 10.1289/EHP9726
Lavigne E, Ryti N, Gasparrini A, Sera F, Weichenthal S, Chen H, To T, Evans GJ, Sun L, Dheri A, Lemogo L, Kotchi SO, Stieb D. Short-term exposure to ambient air pollution and individual emergency department visits for COVID-19: a case-crossover study in Canada. Thorax. 2022 Mar 31:thoraxjnl-2021-217602. doi: 10.1136/thoraxjnl-2021-217602
Razzaq A, Cui Y, Irfan M, Maneengam A, Acevedo-Duque Á. Asymmetric effects of fine particulate matter and stringency policy
on COVID-19 intensity. Int J Environ Health Res. 2022 Mar 31:1-13. doi: 10.1080/09603123.2022.2059452
This study looked at the ICU admissions for COVID 19 as a marker of pandemic transmission in the community. A positive correlation is found between PM2.5 concentration and cases, indicating that the pollution is facilitating the transmission.
Lolli S, Chen YC, Wang SH, Vivone G. Impact of meteorological conditions and air pollution on COVID-19 pandemic transmission in Italy. Sci Rep. 2020 Oct 1;10(1):16213. doi: 10.1038/s41598-020-73197-8. PMID: 33004925
More evidence air pollution causes autoimmune diseases like rheumatoid arthritis, inflammatory bowel disease, and connective tissue disorders
Adami G, Pontalti M, Cattani G, et al Association between long-term exposure to air pollution and immune-mediated diseases: a population-based cohort study RMD Open 2022;8:e002055. doi: 10.1136/rmdopen-2021-002055
Ding S, Sun S, Ding R, Song S, Cao Y, Zhang L. Association between exposure to air pollutants and the risk of inflammatory bowel diseases visits. Environ Sci Pollut Res Int. 2021 Oct 20. doi: 10.1007/s11356-021-17009-0
Xie S, Zhang C, Zhao J, Li D, Chen J. Exposure to concentrated ambient PM2.5 (CAPM) induces intestinal disturbance via inflammation and alternation of gut microbiome. Environ Int. 2022 Feb 14;161:107138. doi: 10.1016/j.envint.2022.107138
Ozone is harmful to the skin, specifically on the statum corneum extracellular matrix of the skin.
Petracca B, Nădăban A, Eeman M, Gooris GS, Bouwstra JA. Effects of ozone on stratum corneum lipid integrity and assembly.
Chem Phys Lipids. 2021 Aug 2:105121. doi: 10.1016/j.chemphyslip.2021.105121. Epub ahead of print. PMID: 34352254.
Particulate pollution damages the cells of the cornea and conjunctiva of the eye.
Hyun SW, Song SJ, Park B, Lee TG, Kim CS. Toxicological effects of urban particulate matter on corneal and conjunctival epithelial cells. Toxicol Res. 2020 Feb 10;36(4):311-318. doi: 10.1007/s43188-019-00034-0. eCollection 2020 Oct. PMID: 33005590
Increasing air pollution increases income inequality and that general government public-health expenditures are an important transmission channel by which air pollution affects income inequality.
Wu J, Pu Y. Air pollution, general government public-health expenditures and income inequality: Empirical analysis based on the spatial Durbin model. PLoS One. 2020 Oct 1;15(10):e0240053. doi: 10.1371/journal.pone.0240053. eCollection 2020. PMID: 33002068 Free PMC article.
Air pollution has an adverse effect on male reproductive health, damaging the DNA in sperm and reducing sperm quality.
Kumar S, Sharma A, Thaker R. Air pollutants and impairments of male reproductive health-an overview. Rev Environ Health. 2021 Jan 29. doi: 10.1515/reveh-2020-0136. Online ahead of print
Zhao Y, Zhu Q, Lin J, Cai J. Association of Exposure to Particulate Matter Air Pollution With Semen Quality Among Men in China. JAMA Netw Open. 2022 Feb 1;5(2):e2148684. doi: 10.1001/jamanetworkopen.2021.48684. PMID: 35175344
Air pollution exposure correlates with rates of anemia in children.
Bora K. Air Pollution as a Determinant of Undernutrition Prevalence among Under-Five Children in India: An Exploratory Study. J Trop Pediatr. 2021 Oct 6;67(5):fmab089. doi: 10.1093/tropej/fmab089
Particles “aged” in the atmosphere may be more toxic than “fresh” particulate pollution.
Offer S, et al. Effect of Atmospheric Aging on Soot Particle Toxicity in Lung Cell Models at the Air-Liquid Interface: Differential Toxicological Impacts of Biogenic and Anthropogenic Secondary Organic Aerosols (SOAs). Environ Health Perspect. 2022 Feb;130(2):27003. doi: 10.1289/EHP9413. Epub 2022 Feb 3. PMID: 35112925
Long term exposure to sulfur dioxide pollution, SOx, is associated with increased risk of osteoporosis related fractures.
Heo S, Kim H, Kim S, Choe SA, Byun G, Lee JT, Bell ML. Associations between Long-Term Air Pollution Exposure and Risk of Osteoporosis-Related Fracture in a Nationwide Cohort Study in South Korea. Int J Environ Res Public Health. 2022 Feb 19;19(4):2404. doi: 10.3390/ijerph19042404.PMID: 3520659
“Crosstalk” occurs between the respiratory and gastrointestinal tracts, commonly referred to as the gut-lung axis. Via microbial secretions, metabolites, immune mediators and lipid profiles, these two organ systems can influence each other. There is early evidence that probiotics, probiotics, and synbiotics may mitigate the negative effects of air pollution.
Keulers L, et al. Probiotics, prebiotics, and synbiotics to prevent or combat air pollution consequences: The gut-lung axis. Environ Pollut. 2022 Feb 28:119066. doi: 10.1016/j.envpol.2022.119066. Online ahead of print. PMID: 35240267 Review
Air filtration leads to increased protein synthesis and enhanced
mitochondrial efficiency, resulting in a highly significant triggering of ATP synthesis and a reduction in oxidative damage.
Antuña E, Carlos Bermejo-Millo J, Caso-Onzain E, Caso-Peláez E, Potes Y, Coto-Montes A. Removal of Environmental Nanoparticles Increases Protein Synthesis and Energy Production in Healthy Humans. Front Bioeng Biotechnol. 2022 Feb 14;10:800011. doi: 10.3389/fbioe.2022.800011. eCollection 2022
The risk of benign brain tumors is increased with air pollution.
Chang KH, Teng CJ, Hsu YC, Tsai SC, Lin HJ, Hsieh TL, Muo CH, Hsu CY, Chou RH. Long-Term Exposure to Air Pollution Associates the Risk of Benign Brain Tumor: A Nationwide, Population-Based, Cohort Study in Taiwan. Toxics. 2022 Apr 2;10(4):176. doi: 10.3390/toxics10040176.PMID: 35448437
More evidence of the penetration of pollution nanoparticles (NP) into human brains. Early life NP exposures pose high risk to brains for development of lethal neurologic outcomes.
Calderón-Garcidueñas L, González-Maciel A, Reynoso-Robles R, Silva-Pereyra HG, Torres-Jardón R, Brito-Aguilar R, Ayala A, Stommel EW, Delgado-Chávez R.Environmentally Toxic Solid Nanoparticles in Noradrenergic and Dopaminergic Nuclei and Cerebellum of Metropolitan Mexico City Children and Young Adults with Neural Quadruple Misfolded Protein Pathologies and High Exposures to Nano Particulate Matter. Toxics. 2022 Mar 29;10(4):164. doi: 10.3390/toxics10040164.PMID: 35448425
Despite being a “criteria” pollutant, and regulated by the EPA, carbon monoxide has received little attention from researchers and from regulators. This large international study however showed that, like PM2.5 and ozone, carbon monoxide is deadly, even at low doses, there is no safe level of carbon monoxide, and that the dose response curve is even steeper at low concentrations, below the EPA’s standards.
Chen K, et al. Ambient carbon monoxide and daily mortality: a global time-series study in 337 cities. The Lancet Planetary Health, 2021; 5 (4): e191 DOI: 10.1016/S2542-5196(21)00026-7
This study from 398 cities in 22 countries showed nitrogen oxides was a risk factor for death from cardiovascular and respiratory diseases, separate, and in addition to, particulate pollution and ozone. And like with the other components of pollution, there is no safe level.
Meng X, et al. Short term associations of ambient nitrogen dioxide with daily total, cardiovascular, and respiratory mortality: multilocation analysis in 398 cities. BMJ 2021; 372 doi: https://doi.org/10.1136/bmj.n534 (Published 24 March 2021)
More evidence of air pollution causing increases in hospitalizations, including at very low concentrations, and especially among the elderly.
Yazdi MD, et al. Long-Term Association of Air Pollution and Hospital Admissions Among Medicare Participants Using a Doubly Robust Additive Model. Circulation, 2021; DOI: 10.1161/CIRCULATIONAHA.120.050252
The smaller the pollution particles the more dangerous they are. This study confirmed that loss of life expectancy from inhalation of PM1 is greater than from PM2.5.
Zheng H, Yi W, Ding Z, Xu Z, Ho HC, Cheng J, Hossain MZ, Song J, Fan Y, Ni J, Wang Q, Xu Y, Wei J, Su H. Evaluation of life expectancy loss associated with submicron and fine particulate matter (PM1 and PM2.5) air pollution in Nanjing, China. Environ Sci Pollut Res Int. 2021 Jul 15. doi: 10.1007/s11356-021-15244-z. Epub ahead of print. PMID: 34268691.
Particulate pollution can simultaneously stimulate bone resorption and halt bone formation. More evidence that air pollution is associated with increased risk of developing osteoporosis
Adami G, Cattani G, Rossini M, Viapiana O, Olivi P, Orsolini G, Bertoldo E, Fracassi E, Gatti D, Fassio A. Association between exposure to fine particulate matter and osteoporosis: a population-based cohort study. Osteoporos Int. 2021 Jul 15. doi: 10.1007/s00198-021-06060-9. Epub ahead of print. PMID: 34268604.
In a heavily polluted city in Iran particulate pollution was associated with a loss of life expectancy of 3 years.
Moradi M, Hadei M, Yazdani M, Goudarzi M, Baboli Z, Tahmasebi Birgani Y, Neisi A, Goudarzi G. Effect of long-term exposure to PM2.5 on years of life lost in a populated Middle Eastern city. Environ Geochem Health. 2021 Feb 5. doi: 10.1007/s10653-021-00827-z. Epub ahead of print. PMID: 33544269.
Evidence is emerging that air pollution is also associatied with kidney. Here is one of the first studies to show that.
Li G, Huang J, Wang J, Zhao M, Liu Y, Guo X, Wu S, Zhang L. Long-Term Exposure to Ambient PM2.5 and Increased Risk of CKD Prevalence in China. J Am Soc Nephrol. 2021 Feb;32(2):448-458. doi: 10.1681/ASN.2020040517. Epub 2020 Dec 17. PMID: 33334736; PMCID: PMC8054885.
Research of the Month: Dec. 6, 2020
Air Pollution and COVID-19
Several papers have been published in the last few months showing that particulate pollution increases severity and lethality of COVID and its transmissibility from one person to another. Here are some of those studies and their conclusions. For example, across more than 3000 counties of the United States, an increase of 1 μg/m3 in PM(2.5) has been shown to increase mortality from COVID-19 by 8%, and in New York state alone, by 15%. Conticini E, Frediani B, Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ Pollut. 2020 Apr 4:114465. doi: 10.1016/j.envpol.2020.114465.
Karan A, Ali K, Teelucksingh S, Sakhamuri S. The impact of air pollution on the incidence and mortality of COVID-19. Glob Health Res Policy. 2020 Sep 1;5:39. doi: 10.1186/s41256-020-00167-y. eCollection 2020. PMID: 32879902 Free PMC article
Cazzolla Gatti R, Velichevskaya A, Tateo A, Amoroso N, Monaco A.Machine learning reveals that prolonged exposure to air pollution is associated with SARS-CoV-2 mortality and infectivity in Italy. Environ Pollut. 2020 Aug 21;267:115471. doi: 10.1016/j.envpol.2020.115471. PMID: 32882464
This study found that COVID-19 pandemic transmission is facilitated by dry and cool environmental conditions and polluted air.
Lolli S, Chen YC, Wang SH, Vivone G. Impact of meteorological conditions and air pollution on COVID-19 pandemic transmission in Italy. Sci Rep. 2020 Oct 1;10(1):16213. doi: 10.1038/s41598-020-73197-8.
Brain
This study was done in Salt Lake County and found that our frequent spikes in particulate pollution are associated with worse math and english scores in grade school students. This is consistent with other studies showing acutely impaired memory and cognition with air pollution. But perhaps the most interesting finding was that the impact was worse among those students of greater socio-economic advantage.
Mullen C, et al. Effects of PM2.5 on Third Grade Students’ Proficiency in Math and English Language Arts. Int. J. Environ. Res. Public Health 2020, 17(18), 6931; https://doi.org/10.3390/ijerph17186931
More evidence that even short-term increase in PM2.5, PM10, NO2, SO2 and O3 concentrations was significantly associated with exacerbation of mental disorders, impaired brain development and other manifestations of neurotoxicity
Lu P, Zhang Y, Xia G, Zhang W, Xu R, Wang C, Guo Y, Li S. Attributable risks associated with hospital outpatient visits for mental disorders due to air pollution: A multi-city study in China. Environ Int. 2020 Jun 30;143:105906. doi: 10.1016/j.envint.2020.105906. [Epub ahead of print]
Lu P, et al. Attributable risks associated with hospital outpatient visits for mental disorders due to air pollution: A multi-city study in China. Environ Int. 2020 Jun 30;143:105906. doi: 10.1016/j.envint.2020.105906. [Epub ahead of print]
Zhao T, et al. Depression and Anxiety With Exposure to Ozone and Particulate Matter: An Epidemiological Claims Data Analysis. J Hyg Environ Health. 2020 May 19;228:113562. doi: 10.1016/j.ijheh.2020.113562. Online ahead of print.
Bronstein J, et al. Diesel exhaust extract exposure induces neuronal toxicity by disrupting autophagy. Toxicological Sciences, 2020; DOI: 10.1093/toxsci/kfaa055
Patten K, et al. Effects of early life exposure to traffic-related air pollution on brain development in juvenile Sprague-Dawley rats. Translational Psychiatry, 2020; 10 (1) DOI: 10.1038/s41398-020-0845-3
Another study that shows metallic air pollution nanoparticles are embedded in the brain even in child, adolescents, and young adults.
Caldero ́n-Garciduen~L, et al. Quadruple abnormal protein aggregates in brainstem pathology and exogenous metal-rich magnetic nanoparticles (and engineered Ti-rich nanorods). The substantia nigrae is a very early target in young urbanites and the gastrointestinal tract a key brainstem portal. Environmental Research 191 (2020) 110139More evidence that air pollution is associated with the pathologic hallmarks of Alzheimer’s.
Iaccarino L, et al. Association Between Ambient Air Pollution and Amyloid Positron Emission Tomography Positivity in Older Adults With Cognitive Impairment. JAMA Neurol. Published online November 30, 2020. doi:10.1001/jamaneurol.2020.3962
Pregnancy and fetal development
Several new studies add to the evidence that air pollution increases the risk of pregnancy complications and poor outcomes, and impaired fetal development
Tran K, et al. Residential Proximity to Oil and Gas Development and Birth Outcomes in California: A Retrospective Cohort Study of 2006–2015 Births. Environmental Health Perspectives, 2020; 128 (6): 067001 DOI: 10.1289/EHP5842
Sarizadeh R, Dastoorpoor M, Goudarzi G, Simbar M. The Association Between Air Pollution and Low Birth Weight and Preterm Labor in Ahvaz, Iran.
Int J Womens Health. 2020 May 4;12:313-325. doi: 10.2147/IJWH.S227049. eCollection 2020. PMID: 32440227 [Pub
Fong KC, Shi L, Papatheodorou S, Di Q, Just A, Kosheleva A, Messerlian C, Schwartz JD. Prenatal exposure to particulate air pollution and gestational age at delivery in Massachusetts neonates 2001-2015: A perspective of causal modeling and health disparities. Environ Epidemiol. 2020 Sep 14;4(5):e113. doi: 10.1097/EE9.0000000000000113. eCollection 2020 Oct.
PMID: 33154990 Free PMC article.
Zanini MJ, et al. Urban-Related Environmental Exposures during Pregnancy and Placental Development and Preeclampsia: a Review. Curr Hypertens Rep. 2020 Sep 3;22(10):81. doi: 10.1007/s11906-020-01088-4.
PMID: 32880755 Review
Heart
This study looks at the pathophysiology and mechanism of how PM 2.5 causes cardio-toxicity. Analyzes specifically the role of a microRNA on PM2.5-and the pathway taken to induce myocardial inflammation and cardiac dysfunction. PM2.5 caused myocardial damage via interstitial edema, inflammatory cell infiltration, and myocardial fiber destruction.
Feng L, Wei J, Liang S, Sun Z, Duan J. miR-205/IRAK2 signaling pathway is associated with urban airborne PM2.5-induced myocardial toxicity.
Nanotoxicology. 2020 Sep 3:1-15. doi: 10.1080/17435390.2020.1813824. Online ahead of print. PMID: 32880505Another study showing that air pollution increases the risk of heart attack
Cramer J, et al. Long-Term Exposure to Air Pollution and Incidence of Myocardial Infarction: A Danish Nurse Cohort Study. Environ Health Perspect. 2020 May;128(5):57003. doi: 10.1289/EHP5818. Epub 2020 May 6.
Lungs
Bronchiectasis is a less common lung disease than asthma or COPD. It is a condition where the bronchi of the lungs are permanently damaged, widened, and thickened. These damaged air passages allow bacteria and mucus to build up and pool in your lungs. This results in frequent infections and blockages of the airways. Daily hospitalizations for bronchiectasis are correlated with multiple types of pollution– particulate matter, sulfur dioxide, nitrogen dioxide, carbon monoxide, ozone, and daily hospitalizations for bronchiectasis.
Wang Z, et al. Association of hospital admission for bronchiectasis with air pollution: A province-wide time-series study in southern China.
Int J Hyg Environ Health. 2020 Nov 3;231:113654. doi: 10.1016/j.ijheh.2020.113654. Online ahead of print. PMID: 33157415
Miscellaneous
This study draws a correlation between air pollution and “frailty” in the elderly. Paper says that when adjusted for age, sex, smoking, urbanity, frail and status changes were significantly associated with high PM 2.5 exposure.
Lee WJ, Liu CY, Peng LN, Lin CH, Lin HP, Chen LK. PM2.5 air pollution contributes to the burden of frailty. Sci Rep. 2020 Sep 2;10(1):14478. doi: 10.1038/s41598-020-71408-w.Air pollution fell in California fell with the COVID 19 lockdown. Authors found a sudden drop in air pollution when the shutdown started and uptick of air pollution when reopening occured. Ground-based observations around California show a 38%, 49%, and 31% drop in the concentration of NO2, carbon monoxide (CO) and particulate matter 2.5 (PM2.5) during the lockdown (March 19-May 7) compared to before (January 26-March 18) in 2020.
Liu Q, et al. Spatiotemporal impacts of COVID-19 on air pollution in California, USA. Sci Total Environ. 2020 Aug 10;750:141592. doi: 10.1016/j.scitotenv.2020.141592.
Air pollution causes disruption of corneal and conjunctival epithelium by decreasing cell viability, altering cell cycle, disrupting mucin, and regulating inflammatory mediators.
Hyun SW, Song SJ, Park B, Lee TG, Kim CS. Toxicological effects of urban particulate matter on corneal and conjunctival epithelial cells. Toxicol Res. 2020 Feb 10;36(4):311-318. doi: 10.1007/s43188-019-00034-0. eCollection 2020 Oct. PMID: 33005590
This study looks at the social impacts and public health consequences of poor air quality. Authors found that ncreasing air pollution increases income inequality and that general government public-health expenditures are an important transmission channel by which air pollution affects income inequality.
Wu J, Pu Y. Air pollution, general government public-health expenditures and income inequality: Empirical analysis based on the spatial Durbin model. PLoS One. 2020 Oct 1;15(10):e0240053. doi: 10.1371/journal.pone.0240053. eCollection 2020.
PMID: 33002068
In the state of Washington, each week of wildfire smoke exposures were estimated to cause 91 cases of increased all-cause mortality, 19.9 increased cardiovascular disease deaths, and 9.7 increased respiratory disease deaths. As climate change gets worse, the negative impacts of smoke will plague the Wasatch front more and more.
Liu Y, Austin E, Xiang J, Gould T, Larson T, Seto E. Health Impact Assessment of PM 2.5 attributable mortality from the September 2020 Washington State Wildfire Smoke Episode. medRxiv. 2020 Sep 22:2020.09.19.20197921. doi: 10.1101/2020.09.19.20197921. Preprint. PMID: 32995819 Free PMC article.
No surprise here. Ambulance dispatches increase during wildfire season.
Yao J, et al. Sub-Daily Exposure to Fine Particulate Matter and Ambulance Dispatches during Wildfire Seasons: A Case-Crossover Study in British Columbia, Canada. Environmental Health Perspectives, 2020; 128 (6): 067006 DOI: 10.1289/EHP5792
More evidence that air pollution causes an increase in community deaths.
Wu X, et al. Evaluating the Impact of Long-term Exposure to Fine Particulate Matter on Mortality Among the Elderly. Science Advances, 2020 DOI: 10.1126/sciadv.aba5692
Yang J, et al. Fine particulate matter constituents and cause-specific mortality in China: A nationwide modelling study. Environ Int. 2020 Jun 30;143:105927. doi: 10.1016/j.envint.2020.105927. [Epub ahead of print]
Daellenbach, KR, et al. Sources of particulate-matter air pollution and its oxidative potential in Europe. Nature, 2020; 587 (7834): 414 DOI: 10.1038/s41586-020-2902-8
Another study showing that air pollution increases the risk of type II diabetes
Elbarbary M, et al. Ambient air pollution exposure association with diabetes prevalence and glycosylated hemoglobin (HbA1c) levels in China. Cross-sectional analysis from the WHO study of AGEing and adult health wave. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2020 Jul 2:1-14. doi: 10.1080/10934529.2020.1787011
Cancer
This Denmark study found more evidence that air pollution causes leukemia, this time in adults.
Taj T, et al. Exposure to PM2.5 constituents and risk of adult leukemia in Denmark: A population-based case-control study. Environ Res. 2020 Nov 3:110418. doi: 10.1016/j.envres.2020.110418. Online ahead of print. PMID: 33157111
The study provides more evidence that pollution decreases survival in cancer patients.
Ou JY, Kirchhoff AC, Hanson HA. Air Pollution across the Cancer Continuum: Extending Our Understanding of the Relationship between Environmental Exposures and Cancer. Cancer Epidemiol Biomarkers Prev. 2020 Oct;29(10):1876-1879. doi: 10.1158/1055-9965.EPI-19-1588.
PMID: 33004409
More evidence that air pollution increases the risk of birth anomalies like neural tube defects
Ravindra K, Chanana N, Mor S. Exposure to air pollutants and risk of congenital anomalies: A systematic review and metaanalysis. Sci Total Environ. 2020 Oct 7:142772. doi: 10.1016/j.scitotenv.2020.142772.
Zhang JY, et al. Maternal exposure to ambient levels of sulfur dioxide and risk of neural tube defects in 14 cities in Liaoning province, China: a population-based case-control study. J Expo Sci Environ Epidemiol. 2020 Oct 1. doi: 10.1038/s41370-020-00273-6. Online ahead of print.
PMID: 33005007
Research of the Month: May 5, 2020
This study has not yet been peer reviewed. But it’s a nationwide study from researchers at the Harvard School of Public Health. It shows that just 1ug/m3 of PM2.5 increases the risk of death from COVID-19, 8%. Given that the annual PM2.5 standard is 12 ug/m3, that means that “acceptable” levels of air pollution would increase the risk of death from COVID-19 nearly 100%.
https://projects.iq.harvard.edu/covid-pm
Another study was done in Italy that showed 78% of the deaths from COVID-19 occurred in the parts of the country with the highest levels of NOx pollution.
Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Science of The Total Environment. Volume 726, 15 July 2020, 138605
Prenatal air pollution exposure is associated with higher blood pressure in childhood.
Rosa MJ, et al. Identifying critical windows of prenatal particulate matter (PM2.5) exposure and early childhood blood pressure. Environ Res. 2019 Dec 23;182:109073. doi: 10.1016/j.envres.2019.109073. [Epub ahead of print]
More evidence of air pollution’s neurotoxic effect, in this case impairing episodic memory.
Petkus AJ, et al. Exposure to fine particulate matter and temporal dynamics of episodic memory and depressive symptoms in older women. Environ Int. 2019 Dec 24;135:105196. doi: 10.1016/j.envint.2019.105196. [Epub ahead of print]
Not only are NOx, SO2, and particulate pollution associated with increased risk of stroke, the relationship between ozone and stroke was “V” shaped, meaning that low concentrations of O3 had a greater association with stroke than moderate concentrations.
Wang Z, et al. Association between short-term exposure to air pollution and ischemic stroke onset: a time-stratified case-crossover analysis using a distributed lag nonlinear model in Shenzhen, China. Environ Health. 2020 Jan 2;19(1):1. doi: 10.1186/s12940-019-0557-4.
Another study showing a higher risk of arthritis with exposure to air pollution.
Yamamoto SS, et al. Household air pollution and arthritis in low-and middle-income countries: Cross-sectional evidence from the World Health Organization’s study on Global Ageing and Adult Health.PLoS One. 2019 Dec 27;14(12):e0226738. doi: 10.1371/journal.pone.0226738. eCollection 2019.
Air pollution is associated with reduced bone mineral density, even in young people, increasing the risk of later on osteoporosis.
Ranzani OT, et al. Association of Ambient and Household Air Pollution With Bone Mineral Content Among Adults in Peri-urban South India. JAMA Netw Open. 2020 Jan 3;3(1):e1918504. doi: 10.1001/jamanetworkopen.2019.18504.
Approximately 30% of lung cancer is precipitated by air pollution.
Santibáñez-Andrade M, et al. Deciphering the Code between Air Pollution and Disease: The Effect of Particulate Matter on Cancer Hallmarks. Int J Mol Sci. 2019 Dec 24;21(1). pii: E136. doi: 10.3390/ijms21010136.More evidence of air pollution provoking lung cancer
Liang D, et al. Lung Cancer in Never-Smokers: A Multicenter Case-Control Study in North China. Front Oncol. 2019 Dec 10;9:1354. doi: 10.3389/fonc.2019.01354. eCollection 2019.Wang Z, et al. Traffic-related environmental factors and childhood obesity: A systematic review and meta-analysis. Obes Rev. 2020 Jan 30. doi: 10.1111/obr.12995. [Epub ahead of print]
Air pollution from solid fuel combustion (wood and coal) increases the risk of breast and cervical cancer mortality.
Liu T, et al. Solid fuel use for heating and risks of breast and cervical cancer mortality in China. Environ Res. 2020 Apr 28;186:109578. doi: 10.1016/j.envres.2020.109578. [Epub ahead of print]
Air pollution is associated with gastric cancer. That is not surprising given that air pollution particles are not just inhaled, but also swallowed.
Yin J, et al. Impact of environmental factors on gastric cancer: A review of the scientific evidence, human prevention and adaptation. J Environ Sci (China). 2020 Mar;89:65-79. doi: 10.1016/j.jes.2019.09.025. Epub 2019 Nov 4.
Brake dust is a significant component of traffic related air pollution. At least regarding the lung, it appears to be as toxic as tail pipe emissions.
Selley L, et al. Brake dust exposure exacerbates inflammation and transiently compromises phagocytosis in macrophages. Metallomics. DOI: 10.1039/c9mt00253g
Nitrogen oxide exposure during childhood increases the risk of later on schizophrenia.
Horsdal H, et al. Association of Childhood Exposure to Nitrogen Dioxide and Polygenic Risk Score for Schizophrenia With the Risk of Developing Schizophrenia. JAMA Network Open, 2019; 2 (11): e1914401 DOI: 10.1001/jamanetworkopen.2019.14401
More evidence that air pollution is toxic to genes and decreases the length of telomeres.
Ma Y, et al. Effect of combustion-derived particles on genotoxicity and telomere length: a study on human cells and exposed populations. Toxicol Lett. 2020 Jan 7. pii: S0378-4274(20)30002-3. doi: 10.1016/j.toxlet.2020.01.002. [Epub ahead of print]
This study showed an increased effect of air pollution on cognition in elderly women compared with men of equal age.
Kim H, et al. Gender Difference in the Effects of Outdoor Air Pollution on Cognitive Function Among Elderly in Korea. Front Public Health. 2019 Dec 10;7:375. doi: 10.3389/fpubh.2019.00375. eCollection 2019.
Air pollution exposure at the time of conception is associated with an increase in a certain type of birth defect of the urethra.
Huang C, et al. Periconceptional exposure to air pollution and congenital hypospadias among full-term infants. Environ Res. 2020 Jan 17;183:109151. doi: 10.1016/j.envres.2020.109151. [Epub ahead of print]
As early as childhood, air pollution exposure demonstrates anatomic changes in the brain, specifically reduced gray matter and cortical thickness.
Beckwith T, et al. Reduced gray matter volume and cortical thickness associated with traffic-related air pollution in a longitudinally studied pediatric cohort. PLOS ONE, 2020; 15 (1): e0228092 DOI: 10.1371/journal.pone.0228092
Small increases in air pollution are followed within hours by an increase in the risk of heart attacks.
Chen K, et al. Hourly Exposure to Ultrafine Particle Metrics and the Onset of Myocardial Infarction in Augsburg, Germany. Environmental Health Perspectives, 2020; 128 (1): 017003 DOI: 10.1289/EHP5478
Air pollution alters the composition and functional profile of the bacterial population of the GI tract. This is likely one explanation for the growing evidence that air pollution increases the risk of inflammatory bowel disease.
Fouladi F, et al. Air pollution exposure is associated with the gut microbiome as revealed by shotgun metagenomic sequencing. Environment International, 2020; 138: 105604 DOI: 10.1016/j.envint.2020.105604
Grande G, et al. Association Between Cardiovascular Disease and Long-term Exposure to Air Pollution With the Risk of Dementia. JAMA Neurology, 2020; DOI: 10.1001/jamaneurol.2019.4914
This fascinating study found that air pollution levels closer to the ground, at the height where a baby would sit in a stroller, are 44% higher than the levels a few feet higher, i.e. where the parents pushing the stroller would be inhaling.
Sharma A, et al. Quantification of air pollution exposure to in-pram babies and mitigation strategies. Environment International, 2020; 139: 105671 DOI: 10.1016/j.envint.2020.105671
Air pollution exposure to a pregnant mother during the first trimester, PM2.5 of 6.5 ug/m3, was associated with a 17% increased risk of the baby having autism, but only in boys.
Jo H, et al. Sex-specific associations of autism spectrum disorder with residential air pollution exposure in a large Southern California pregnancy cohort. Environmental Pollution, Volume 254, Part A, November 2019, 113010
Chronic air pollution is associated with calcification of the coronary arteries in asymptomatic adults.
Huynh Q, et al. Long-term exposure to ambient air pollution is associated with coronary artery calcification among asymptomatic adults. Eur Heart J Cardiovasc Imaging. 2020 May 1. pii: jeaa073. doi: 10.1093/ehjci/jeaa073. [Epub ahead of print]
This study analyzed the air pollution reduction as a result of the contraction of economic activity in China and assessed how many lives might have been saved compared to the lives lost from COVID-19. The researchers concluded that the health benefits and reduced mortality secondary to less air pollution was greater than the number of deaths from the coronavirus.
Chen K, Wang M, Huang C, Kinney PL, Anastas PT. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China [published online ahead of print, 2020 May 13]. Lancet Planet Health. 2020;doi:10.1016/S2542-5196(20)30107-8
More evidence that air pollution impairs cognitive performance.
Yu X, et al. Exposure to air pollution and cognitive impairment risk: a meta-analysis of longitudinal cohort studies with dose-response analysis. J Glob Health. 2020 Jun;10(1):010417. doi: 10.7189/jogh.10.010417.
This study strengthens the evidence that air pollution is a significant risk factor for pre-term birth.
Zhang X, et al. Maternal PM<sub>2.5</sub> exposure triggers preterm birth: a cross-sectional study in Wuhan, China. Glob Health Res Policy. 2020 May 1;5:17. doi: 10.1186/s41256-020-00144-5. eCollection 2020.
Prenatal air pollution increases the risk of reproductive birth defects.
Sun X, et al. Prenatal exposure to residential PM<sub>2.5</sub> and anogenital distance in infants at birth: A birth cohort study from Shanghai, China. Environ Pollut. 2020 Apr 27;264:114684. doi: 10.1016/j.envpol.2020.114684. [Epub ahead of print]
For patients that end up in the ICU, there is an increased risk of mortality with more air pollution. Specifically, the risk of death was increased 18% per increase of 10 ug/m3 of PM2.5.
Groves CP, et al. Intensive care admissions and outcomes associated with short-term exposure to ambient air pollution: a time series analysis. Intensive Care Med. 2020 Apr 30. doi: 10.1007/s00134-020-06052-z. [Epub ahead of print]
Research of the Month: Dec. 23, 2019
Published in one of the most prestigious medical journals, this study of 4.5 million US veterans found that 99% of the deaths related to air pollution occur in populations where the air pollution meets the EPA’s standards. This puts a definitive stamp on the concept that there is no safe level of air pollution, and that those standards, which are supposed to be updated every 5 years, are far too lax. Also, nine causes of death related to air pollution were identified, including causes not previous connected to air pollution—kidney disease, dementia, and type II diabetes.
Bowe B, et al. Burden of Cause-Specific Mortality Associated With PM2.5 Air Pollution in the United States. JAMA Network Open. November 20, 2019
This meta-analysis strengthens the evidence that PM2.5 is associated with hypertensive disorders of pregnancy.
Sun M, et al. The correlation between PM<sub>2.5</sub> exposure and hypertensive disorders in pregnancy: A Meta-analysis. Sci Total Environ. 2019 Nov 2;703:134985. doi: 10.1016/j.scitotenv.2019.134985. [Epub ahead of print]
More evidence that air pollution increases the risk of premature rupture of membranes, a disorder that puts both the baby and mother at risk for infection, and for premature birth.
Wang K, et al. Maternal exposure to ambient fine particulate matter and risk of premature rupture of membranes in Wuhan, Central China: a cohort study. Environ Health . 2019 Nov 14;18(1):96. doi: 10.1186/s12940-019-0534-y.
This is a meta-analysis that demonstrates the hard evidence that air pollution contributes to gestational diabetes.
Hu CY, et al. Human epidemiological evidence about the association between air pollution exposure and gestational diabetes mellitus: Systematic review and meta-analysis. Environ Res. 2019 Oct 21;180:108843. doi: 10.1016/j.envres.2019.108843. [Epub ahead of print]
More evidence that ozone, once thought to be a weaker toxin than particulate pollution, is associated with preterm birth and still birth.
Smith RB, et al. Impacts of air pollution and noise on risk of preterm birth and stillbirth in London. Environ Int. 2019 Nov 26;134:105290. doi: 10.1016/j.envint.2019.105290. [Epub ahead of print]
Short term exposure to PM2.5 and risk of hospital admission were found for several prevalent but rarely studied diseases, such as septicemia, fluid and electrolyte disorders, and acute and unspecified renal failure. Positive associations were also found between risk of hospital admission and cardiovascular and respiratory diseases, Parkinson’s disease, diabetes, phlebitis, thrombophlebitis, and thromboembolism.
Mahase E. Study links air pollution to several new causes of hospital admissions.BMJ. 2019 Nov 28;367:l6741. doi: 10.1136/bmj.l6741.
The authors of this study, from the prestigious journal, Chest, describe the impacts of air pollution in nearly the exact terms that UPHE has been using for several years. Air pollution is the world’s fifth leading risk factor for death. Tissue damage may result directly from pollutant toxicity because fine and ultrafine particles can gain access to organs, or indirectly through systemic inflammatory processes. It can harm any organ in the body. Air pollution can harm everyone’s health, but some are more susceptible than others, either because of genetics, socioeconomics, race, or ethnicity. Public health is damaged as levels below those previously considered to be safe.
Schraufnagel D, et al. Air Pollution and Noncommunicable Diseases. Chest. February 2019Volume 155, Issue 2, Pages 409–416
This study demonstrates that the benefits of cleaner air occur almost immediately. Respiratory symptoms, hospitalizations, school absenteeism, and mortality start to drop within a few weeks, although they may not drop back to normal. And there is additional benefit to making already clean air even cleaner.
Schraufnagel D, et al. Health Benefits of Air Pollution Reduction. Annals of the American Thoracic Society. Vol. 16, No. 12 | Dec 01, 2019More evidence that air pollution related mortality is found at concentrations below the EPA’s national standards.
Michael Brauer M, et al. Mortality–Air Pollution Associations in Low-Exposure Environments (MAPLE): Phase 1. Health Effects Institute. Research Report 203, November 2019
This is perhaps the most comprehensive analysis of the major studies exploring the relationship between PM2.5 and morality. It establishes again that increases of 1 ug/m3 of PM2.5 chronic exposure increase community deaths rates about 1%. Acute spikes of PM2.5 will add additional mortality, as will ozone. It is from data like this that UPHE states that between 1,000 and 2,000 people die prematurely every year in Utah because of our air pollution.
Pope CA, et al. Fine particulate air pollution and human mortality: 25+ years of cohort studies. Environmental Research. Available online 14 November 2019, 108924
By promoting inflammation, particulate pollution was found to contribute to rheumatoid and osteoarthritis, higher levels of antibodies, severe bone density decrease, cartilage wear, and structure damages.
Peng K, et al. Particulate matter exposure aggravates osteoarthritis severity.Clin Sci (Lond). 2019 Oct 18. pii: CS20190458. doi: 10.1042/CS20190458. [Epub ahead of print]. PMID: 31696218 [PubMed – as supplied by publisher]
Alex AM, et al. Exposure to ambient air pollution and autoantibody status in rheumatoid arthritis. Clin Rheumatol. 2019 Nov 15. doi: 10.1007/s10067-019-04813-w. [Epub ahead of print]
More evidence that air pollution is associated with sleep disorders, including sleep apnea.
Tang M, et al. The association of short-term effects of air pollution and sleep disorders among elderly residents in China. Sci Total Environ. 2019 Nov 19:134846. doi: 10.1016/j.scitotenv.2019.134846. [Epub ahead of print]
Yu H, et al. The Association between Air Pollution and Sleep Duration: A Cohort Study of Freshmen at a University in Beijing, China. Int J Environ Res Public Health. 2019 Sep 11;16(18). pii: E3362. doi: 10.3390/ijerph16183362.
Many studies have shown that air pollution impairs the normal electrical signaling of the heart. That is one way that air pollution causes sudden death. This study suggests that the effect on heart electrical activity begins in infancy.
Cowell WJ, et al. Prenatal Exposure to PM2.5 and Cardiac Vagal Tone during Infancy: Findings from a Multiethnic Birth Cohort. Environmental Health Perspectives, 2019; 127 (10): 107007 DOI: 10.1289/EHP4434
Inhalation of particulate pollution associated with Mountain Top Removal mining contributes to dramatically increased risk for dementia related mortality.
Salm AK, et al. Increased Dementia Mortality in West Virginia Counties with Mountaintop Removal Mining? Int J Environ Res Public Health. 2019 Nov 4;16(21). pii: E4278. doi: 10.3390/ijerph16214278. PMID: 31689936 [PubMed – in process]
Air pollution changes the physical development of the brain in utero, including reducing the size of certain parts of the brain. In this study, the corpus callosum, the bridge between both hemispheres, was decreased in volume with more air pollution exposure of the pregnant mother. This abnormality is associated with behavioral disorders.
Mortamais M, et al. Effects of prenatal exposure to particulate matter air pollution on corpus callosum and behavioral problems in children. Environ Res. 2019 Sep 7;178:108734. doi: 10.1016/j.envres.2019.108734. [Epub ahead of print]
More evidence that air pollution, prenatal or during infancy, is associated with increased risk of autism.
Jo H, et al. Sex-specific associations of autism spectrum disorder with residential air pollution exposure in a large Southern California pregnancy cohort. Environ Pollut. 2019 Nov;254(Pt A):113010. doi: 10.1016/j.envpol.2019.113010. Epub 2019 Aug 5.
These studies showed that air pollution increased the rate of psychiatric emergency department visits for pediatric and adult patients.
Brokamp C, et al. Psychiatric Emergency Department Utilization and Fine Particulate Matter: A Case-Crossover Study. Environ Health Perspect. 2019 Sep;127(9):97006. doi: 10.1289/EHP4815. Epub 2019 Sep 25. PMID: 31553231 [PubMed – in process] Free Article
Bernardini F, et al. Air pollutants and daily number of admissions to psychiatric emergency services: evidence for detrimental mental health effects of ozone. Epidemiol Psychiatr Sci. 2019 Nov 6:1-7. doi: 10.1017/S2045796019000623. [Epub ahead of print] PMID: 31690359 [PubMed – as supplied by publisher]
Numerous studies have found a correlation between air pollution and behavioral disorders including unethical behavior. This study of over 86 million people found that correlation also exists for violent crime.
Burkhardt J, et al. The effect of pollution on crime: Evidence from data on particulate matter and ozone. Journal of Environmental Economics and Management, 2019; 102267 DOI: 10.1016/j.jeem.2019.102267
More evidence of air pollution’s impact on brain function. For every 2.81 μg/m3 of PM2.5, the annual decline rate in a certain type of memory capability was accelerated by 19.3%.
Younan D, et al. Particulate matter and episodic memory decline mediated by early neuroanatomic biomarkers of Alzheimer’s disease. Brain, awz348, https://doi.org/10.1093/brain/awz348. Published: 20 November 2019
Chronic exposure to more HAPs (hazardous air pollutants) was found to be associated with worse academic performance among school children in reading, math, and science through the third grade.
Grineski S, et al. Hazardous air pollutants are associated with worse performance in reading, math, and science among US primary schoolchildren. Environ Res. 2019 Nov 15:108925. doi: 10.1016/j.envres.2019.108925. [Epub ahead of print]
Air pollution decreases stock market returns by decreasing mood and trading activity among brokers.
Wu Q, et al. Air pollution, stock returns, and trading activities in China. Pacific-Basin Finance Journal. Volume 51, October 2018, Pages 342-365
More evidence that air pollution is associated with increased risk for metabolic disorders like type II diabetes
Holliday KM, et al. Air pollution-associated changes in biomarkers of diabetes risk. Environ Epidemiol. 2019 Aug 13;3(4):e059. doi: 10.1097/EE9.0000000000000059. eCollection 2019 Aug.
Hendryx M, et al. Exposure to heavy metals from point pollution sources and risk of incident type 2 diabetes among women: a prospective cohort analysis. Int J Environ Health Res. 2019 Sep 19:1-12. doi: 10.1080/09603123.2019.1668545. [Epub ahead of print]
Kim JS, et al. Associations of air pollution, obesity and cardiometabolic health in young adults: The Meta-AIR study. Environ Int. 2019 Oct 14;133(Pt A):105180. doi: 10.1016/j.envint.2019.105180. [Epub ahead of print]
Yang BY, et al. Ambient air pollution and diabetes: A systematic review and meta-analysis. Environ Res. 2019 Oct 12;180:108817. doi: 10.1016/j.envres.2019.108817. [Epub ahead of print]
Yu Y, et al. Air pollution, noise exposure, and metabolic syndrome – A cohort study in elderly Mexican-Americans in Sacramento area. Environ Int. 2019 Nov 25;134:105269. doi: 10.1016/j.envint.2019.105269. [Epub ahead of print]
Another study showing that air pollution impairs thyroid function in pregnant mothers, which can, in turn, impair fetal brain development
Ghassabian A, et al. Association of Exposure to Ambient Air Pollution With Thyroid Function During Pregnancy. JAMA Netw Open. 2019 Oct 2;2(10):e1912902. doi: 10.1001/jamanetworkopen.2019.12902.
More studies that show air pollution is associated with higher rates of lung, breast, and nasopharyngeal cancer.
White AJ, et al. Air Pollution, Clustering of Particulate Matter Components, and Breast Cancer in the Sister Study: A U.S.-Wide Cohort. Environ Health Perspect. 2019 Oct;127(10):107002. doi: 10.1289/EHP5131. Epub 2019 Oct 9.
Huang HC, et al. Association between coarse particulate matter (PM10-2.5) and nasopharyngeal carcinoma among Taiwanese men. J Investig Med. 2019 Oct 16. pii: jim-2019-001119. doi: 10.1136/jim-2019-001119. [Epub ahead of print]
Goldberg MS, et al. Associations between incident breast cancer and ambient concentrations of nitrogen dioxide from a national land use regression model in the Canadian National Breast Screening Study. Environ Int. 2019 Oct 21;133(Pt B):105182. doi: 10.1016/j.envint.2019.105182. [Epub ahead of print]
Zhang Z, et al. Association between particulate matter air pollution and lung cancer. Thorax. 2019 Nov 14. pii: thoraxjnl-2019-213722. doi: 10.1136/thoraxjnl-2019-213722. [Epub ahead of print]
Research of the Month: Sept. 7, 2019
Ozone has historically been considered the “weaker sister” of the two high volume pollutants–ozone and particulate matter. But ozone is a powerful oxidizing agent and has been proven to cause a decrease in lung function and damage to lung tissue. Ozone has been associated with almost all the health consequences of particulate matter, if only to a slightly lesser extent.
But this new study shows that the lung is exquisitely sensitive to even small increments of ozone. Researchers followed nearly 7,000 patients and found emphysematous destruction of lung tissue and loss of lung function (measured by CAT scans and spirometry) in both smokers and non-smokers at this shocking rate: Just 3 ppb increase in ozone exposure over ten years caused as much lung damage as smoking a pack a day of cigarettes for 29 years.
Wang M, et al. Association Between Long-term Exposure to Ambient Air Pollution and Change in Quantitatively Assessed Emphysema and Lung Function. JAMA, 2019; 322 (6): 546 DOI: 10.1001/jama.2019.10255
We have seen the emergence of studies showing that particulate matter embedded in the critical organs of virtually all humans. Sixty-five people were studied at autopsy, the average age was 25, the youngest was only three years old. Researchers found between 2 billion and 22 billion nanoparticles of air pollution in embedded in heart tissue itself of all subjects. Those people who had lived in the highly polluted Mexico City had between 2 and 10 ten times as many pollution particles as those that lived less polluted environments.
Calderón-Garcidueñas L, et al. Combustion- and friction-derived magnetic air pollution nanoparticles in human hearts. Environmental Research
Volume 176, September 2019, 108567
Even newborns exposed to more air pollution have higher blood pressure.
Madhloum N. et al. Neonatal blood pressure in association with prenatal air pollution exposure, traffic, and land use indicators: An ENVIRONAGE birth cohort study. Environ Int. 2019 Jun 18;130:104853. doi: 10.1016/j.envint.2019.05.047. [Epub ahead of print]
Numerous studies have shown the toxicity of air pollution to brain function and development, even changing brain architecture. This study show that a critical area of the brain for memory, the hippocampus, is smaller in size in adults exposed to more air pollution.
Hedges DW, et al. Association between Exposure to Air Pollution and Hippocampal Volume in Adults in the UK Biobank. Neurotoxicology. 2019 Jun 17. pii: S0161-813X(19)30053-1. doi: 10.1016/j.neuro.2019.06.005. [Epub ahead of print]
The length of telomeres is a marker of aging at the molecular level. Here is another study showing that air pollution exposure during pregnancy was associated with shorter telomeres measured at the age of eight.
Clemente DBP, et al. Prenatal and Childhood Traffic-Related Air Pollution Exposure and Telomere Length in European Children: The HELIX Project. Environ Health Perspect. 2019 Aug;127(8):87001. doi: 10.1289/EHP4148. Epub 2019 Aug 8.
We have known for several years that the success rate of in vitro fertilization is decreased with more air pollution. This study shows that can be offset by supplemental folic acid.
Gaskins AJ, et al. Exposure to Traffic-Related Air Pollution, Supplemental Folate Intake, and Live Birth Among Women Undergoing Assisted Reproduction. Am J Epidemiol. 2019 Jun 26. pii: kwz151. doi: 10.1093/aje/kwz151. [Epub ahead of print]
Thyroid function is critical to good health at any age, and especially critical for normal fetal development, including brain development. The impact of air pollution on thyroid function has only recently been studied. Two new studies show that air pollution impairs thyroid function in pregnant mothers and in turn impairs fetal thyroid development, which may contribute to the well established connection between air pollution and low birth weight.
Howe CG, et al. Association of Prenatal Exposure to Ambient and Traffic-Related Air Pollution With Newborn Thyroid Function: Findings From the Children’s Health Study. JAMA Network Open, 2018 DOI: 10.1001/jamanetworkopen.2018.2172
Wang X, et al. Evaluation of maternal exposure to PM2.5 and its components on maternal and neonatal thyroid function and birth weight: a cohort study. Thyroid. 2019 Jul 12. doi: 10.1089/thy.2018.0780. [Epub ahead of print]
We have seen numerous studies showing that air pollution exposure early in life (in utero and infancy) can have lasting impacts on health, like heart and lung function, that don’t show up for decades. This study shows early life exposure is even associated with higher rates of arthritis in adulthood, especially rheumatoid arthritis.
Shepherd A, et al. Arthritis diagnosis and early-life exposure to air pollution. Environ Pollut. 2019 Oct;253:1030-1037. doi: 10.1016/j.envpol.2019.07.054. Epub 2019 Jul 13.
Research Paper of the Month: Dec. 15, 2108
We have known for several years that air pollution can harm the developing fetus in utero. We have even had substantial evidence that air pollution affects DNA and gene integrity. But an alarming new study in lab mice starkly shows what air pollution can do to future generations, even if they are never exposed. In mice, merely “pre-conception” exposure to air pollution, and no exposure after conception, at a level only slightly above the EPA’s 24 hour standard for PM2.5, was enough to cause impaired heart function, decreased heart muscle mass, activated an oxidative stress response and triggered systemic inflammation through genetic changes, later on adulthood. The moral to this story is powerful. Even future generations are harmed by the air pollution breathed by future parents.
Tanwar V, et al. Preconception Exposure to Fine Particulate Matter Leads to Cardiac Dysfunction in Adult Male Offspring. Journal of the American Heart Association, 2018; 7 (24) DOI: 10.1161/JAHA.118.010797
Proximity to oil and gas drilling activity (think fracking), increases blood pressure, arterial stiffness, and the chemical markers of inflammation.
McKenziea LM, et al. Relationships between indicators of cardiovascular disease and intensity of oil and natural gas activity in Northeastern Colorado. Environmental Research, Volume 170, March 2019, Pages 56-64.
Two good review articles on how air pollution affects the cardiovascular system.
Hamanaka RB, et al. Particulate Matter Air Pollution: Effects on the Cardiovascular System. Front Endocrinol (Lausanne). 2018 Nov 16;9:680. doi: 10.3389/fendo.2018.00680. eCollection 2018.
Rajagopalan S, et al. Air Pollution and Cardiovascular Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2018 Oct 23;72(17):2054-2070. doi: 10.1016/j.jacc.2018.07.099.
Prenatal exposure to air pollution has profound effect on fetal development. In this case prenatal exposure to cooking stove emissions resulted in decreased lung function and increased risk of pneumonia in infants.
Lee AG, et al. Prenatal Household Air Pollution is Associated with Impaired Infant Lung Function with Sex-Specific Effects: Evidence from GRAPHS, a Cluster Randomized Cookstove Intervention Trial. Am J Respir Crit Care Med. 2018 Sep 26. doi: 10.1164/rccm.201804-0694OC. [Epub ahead of print]
More evidence that air pollution, in this case black carbon and the metal nickel (by products of fossil fuel combustion), impairs cognitive function, specifically, verbal memory, recognition, mental processing speed, and executive function, which all focused in frontal and pre- frontal lobe areas.
Wurth R, et al. Fine Particle Sources and Cognitive Function in An Older Puerto Rican Cohort in Greater Boston. Environ Epidemiol. 2018 Sep;2(3). pii: e022. doi: 10.1097/EE9.0000000000000022.
Proximity to heavily trafficked roads at the time of birth is associated with DNA damage and impaired cognition measured later in childhood.
Peng C, et al. Residential Proximity to Major Roadways at Birth, DNA Methylation at Birth and Midchildhood, and Childhood Cognitive Test Scores: Project Viva(Massachusetts, USA) First Published:18 September 2018097006https://doi.org/10.1289/EHP2034
More evidence that air pollution threatens the integrity of fetal development. This study was done at the University of Utah and showed that over an eight year period, our air pollution increased the risk of miscarriage by 16%.
Leiser CL, et al. Acute effects of air pollutants on spontaneous pregnancy loss: a case-crossover study. Fertility and Sterility, 2018; DOI: 10.1016/j.fertnstert.2018.10.028
More detail on how early life air pollution exposure affects the micro anatomy of the brain, i.e. decreases the number of neurons, alters the blood brain barrier and increases microhemorrhages, all of which were associated with impaired brain function in animals.
Woodward NC, et al. Prenatal and early life exposure to air pollution induced hippocampal vascular leakage and impaired neurogenesis in association with behavioral deficits. Transl Psychiatry. 2018 Nov 29;8(1):261. doi: 10.1038/s41398-018-0317-1.
Another study showing a connection between air pollution and behavioral disorders like ADHD.
Ren Y, et al. Outdoor air pollution pregnancy exposures are associated with behavioral problems in China’s preschoolers. Environ Sci Pollut Res Int. 2018 Nov 22. doi: 10.1007/s11356-018-3715-2. [Epub ahead of print]
Exposure to air pollution is associated with lower verbal scores, white matter is more affected than gray matter, and the effect increases with the duration of exposure. Less well educated men over age 60 are the most vulnerable to this effect.
Zhang X, et al. The impact of exposure to air pollution on cognitive performance. PNAS September 11, 2018 115 (37) 9193-9197; published ahead of print August 27, 2018
A good review of the evidence that air pollution increases the risk of insulin resistance and type II diabetes.
Dang J, et al. Associations of Exposure to Air Pollution with Insulin Resistance: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2018 Nov 20;15(11). pii: E2593. doi: 10.3390/ijerph15112593.
Air pollution is associated with other metabolic disorders like fatty liver disease and an adverse blood lipid profile.
Xu MX, et al. Prolonged PM2.5 exposure elevates risk of oxidative stress-driven nonalcoholic fatty liver disease by triggering increase of dyslipidemia. Free Radic Biol Med. 2018 Nov 19. pii: S0891-5849(18)31447-3. doi: 10.1016/j.freeradbiomed.2018.11.016. [Epub ahead of print]
More studies associating air pollution and risk of stroke and mortality from stroke.
Xue T, et al. A national case-crossover study on ambient ozone pollution and first-ever stroke among Chinese adults: Interpreting a weak association via differential susceptibility. Sci Total Environ. 2018 Nov 6;654:135-143. doi: 10.1016/j.scitotenv.2018.11.067. [Epub ahead of print]
Zhang R, et al. Acute Effects of Particulate Air Pollution on Ischemic Stroke and Hemorrhagic Stroke Mortality. Front Neurol. 2018 Oct 2;9:827. doi: 10.3389/fneur.2018.00827. eCollection 2018.
Tian Y, et al. Association between ambient air pollution and daily hospital admissions for ischemic stroke: A nationwide time-series analysis. PLoS Med. 2018 Oct 4;15(10):e1002668. doi: 10.1371/journal.pmed.1002668. eCollection 2018 Oct.
A review article on all the evidence that air pollution shortens telomeres, which reduces life expectancy.
Miri M, et al. Air pollution and telomere length in adults: A systematic review and meta-analysis of observational studies. Environ Pollut. 2018 Oct 8;244:636-647. doi: 10.1016/j.envpol.2018.09.130. [Epub ahead of print]
Here’s another study showing that air pollution is associated with kidney disease.
Chan TC, et al. Long-Term Exposure to Ambient Fine Particulate Matter and Chronic Kidney Disease: A Cohort Study. Published:15 October 2018CID: 107002https://doi.org/10.1289/EHP3304
We have said many times that not all air pollution is created equal. This study found that stoves that combust various solid fuels, the greatest toxicity to cells, including causing the death of lung cells, was found with burning wood pellets.
Marchetti S, et al. In vitro lung toxicity of indoor PM10 from a stove fueled with different biomasses. Sci Total Environ. 2019 Feb 1;649:1422-1433. doi: 10.1016/j.scitotenv.2018.08.249. Epub 2018 Aug 20.
Just about every type of cancer is provoked by air pollution. This study shows that even cancers thought to be exclusively associated with smoking are caused by air pollution, in this case nasopharyngeal cancer.
Fan HC, et al. Increased risk of incident nasopharyngeal carcinoma with exposure to air pollution. PLoS One. 2018 Sep 28;13(9):e0204568. doi: 10.1371/journal.pone.0204568. eCollection 2018.
Another study showing increases in hospital admissions for respiratory and cardiovascular diseases with more air pollution.
Phosri A, et al. Effects of ambient air pollution on daily hospital admissions for respiratory and cardiovascular diseases in Bangkok, Thailand. Sci Total Environ. 2019 Feb 15;651(Pt 1):1144-1153. doi: 10.1016/j.scitotenv.2018.09.183. Epub 2018 Sep 15.
Research Paper of the Month: Sept. 23, 2018
We know that air pollution affects the heart and blood vessels through multiple mechanisms. Heart attacks causing sudden death is the signature outcome of air pollution exposure. However it was indeed sobering to see this study of almost 4,000 people that showed even in middle aged adults that didn’t have known heart disease, air pollution exposure well below the EPA standards, increased the size of heart chambers, which is indicative of impaired function, and a prelude to heart failure. Extrapolating from this study to the Wasatch Front suggests that our air pollution is responsible for about a 10% increase in the size of our heart chambers.
Aung N, et al. Association Between Ambient Air Pollution and Cardiac Morpho-Functional Phenotypes, insights From the UK Biobank Population Imaging Study. Originally published3 Aug 2018Circulation. 2018;0:CIRCULATIONAHA.118.034856
Resting heart rate is often thought of as a marker, although not a perfect one, of physical fitness. Air pollution is associated with a higher resting heart rate.
Xie X, et al. Long-term exposure to fine particulate matter and tachycardia and heart rate: Results from 10 million reproductive-age adults in China. Environ Pollut. 2018 Aug 11;242(Pt B):1371-1378. doi: 10.1016/j.envpol.2018.08.022. [Epub ahead of print]
More evidence that air pollution is associated with a worse blood lipid profile.
Yang BY, et al. Exposure to ambient air pollution and blood lipids in adults: The 33 Communities Chinese Health Study. Environ Int. 2018 Jul 23;119:485-492. doi: 10.1016/j.envint.2018.07.016. [Epub ahead of print]
Another study showing that air pollution harms brain development in children, in this case through chemical changes in DNA.
Peng C, et al. Residential Proximity to Major Roadways at Birth, DNA Methylation at Birth and Midchildhood, and Childhood Cognitive Test Scores: Project Viva(Massachusetts, USA) Published: 18 September 2018, DOI: https://doi.org/10.1289/EHP2034
Air pollution is associated with increased rates of upper and lower respiratory and ear infections in children.
Kennedy CM, et al. Associations of mobile source air pollution during the first year of life with childhood pneumonia, bronchiolitis, and otitis media. Environ Epidemiol. 2018 Mar;2(1). pii: e007. doi: 10.1097/EE9.0000000000000007.
Multiple new studies showing air pollution causing adverse pregnancy outcomes, including closer proximity to industrial pollution sources associated with low birth weight newborns.
Gong X et al. Associations between maternal residential proximity to air emissions from industrial facilities and low birth weight in Texas, USA. Environ Int. 2018 Aug 7;120:181-198. doi: 10.1016/j.envint.2018.07.045. [Epub ahead of print]
Wang L, et al. Association between early prenatal exposure to ambient air pollution and birth defects: evidence from newborns in Xi’an, China. J Public Health (Oxf). 2018 Aug 18. doi: 10.1093/pubmed/fdy137. [Epub ahead of print]
He T, et al. Ambient air pollution, H19/DMR methylation in cord blood and newborn size: A pilot study in Zhengzhou City, China. Chemosphere. 2018 Aug 30;212:863-871. doi: 10.1016/j.chemosphere.2018.08.140. [Epub ahead of print]
Barn P, et al. The effect of portable HEPA filter air cleaner use during pregnancy on fetal growth: The UGAAR randomized controlled trial. Environ Int. 2018 Sep 10. pii: S0160-4120(18)31141-3. doi: 10.1016/j.envint.2018.08.036. [Epub ahead of print]
Wang Q, et al. Identifying windows of susceptibility for maternal exposure to ambient air pollution and preterm birth. Environ Int. 2018 Sep 18;121(Pt 1):317-324. doi: 10.1016/j.envint.2018.09.021. [Epub ahead of print]
Liu WY, et al. Association between ambient air pollutants and preterm birth in Ningbo, China: a time-series study. BMC Pediatr. 2018 Sep 20;18(1):305. doi: 10.1186/s12887-018-1282-9.
More evidence that air pollution causes DNA damage and increases DNA repair activity.
Ledda C, et al. Mutagenic and DNA repair activity in traffic policemen: a case-crossover study.J Occup Med Toxicol. 2018 Aug 8;13:24. doi: 10.1186/s12995-018-0206-9. eCollection 2018.
A meta-analysis of studies showing air pollution causes shorter telomere length, a marker of accelerated aging, and predictor of premature death.
Zhao B, et al. Air pollution and telomere length: a systematic review of 12,058 subjects. Cardiovasc Diagn Ther. 2018 Aug;8(4):480-492. doi: 10.21037/cdt.2018.06.05.
Air pollution during pregnancy is associated with increased rates of obesity in childhood.
Kim JS, et al. Longitudinal associations of in utero and early life near-roadway air pollution with trajectories of childhood body mass index. Environ Health. 2018 Sep 14;17(1):64. doi: 10.1186/s12940-018-0409-7.
Several new studies showing air pollution’s association with increased risk of cancer–childhood cancers, lung cancer, and cancers of the upper digestive tract and stomach.
Consonni D, et al. Outdoor particulate matter (PM10) exposure and lung cancer risk in the EAGLE study. PLoS One. 2018 Sep 14;13(9):e0203539. doi: 10.1371/journal.pone.0203539. eCollection 2018.
Weinmayr G, et al. Particulate matter air pollution components and incidence of cancers of the stomach and the upper aerodigestive tract in the European Study of Cohorts of Air Pollution Effects (ESCAPE). Environ Int. 2018 Aug 7;120:163-171. doi: 10.1016/j.envint.2018.07.030. [Epub ahead of print]
Ribeiro AG, et al. Incidence and mortality risk for respiratory tract cancer in the city of São Paulo, Brazil: Bayesian analysis of the association with traffic density. Cancer Epidemiol. 2018 Jul 23;56:53-59. doi: 10.1016/j.canep.2018.07.005. [Epub ahead of print]
Seifi M, et al. Exposure to ambient air pollution and risk of childhood cancers: A population-based study in Tehran, Iran. Sci Total Environ. 2018 Jul 24;646:105-110. doi: 10.1016/j.scitotenv.2018.07.219. [Epub ahead of print]
Two new studies showing increased rates of appendicitis with more air pollution.
Aroui H, et al. The effect of environmental factors on the incidence of perforated appendicitis. Ann Ital Chir. 2018 Jul 23;7. pii: S0003469X18028014. [Epub ahead of print]
Chen CC, et al. Effects of ambient air pollution exposure on frequency of hospital admissions for appendicitis in Taipei, Taiwan.J Toxicol Environ Health A. 2018 Jul 26:1-7. doi:10.1080/15287394.2018.1498276. [Epub ahead of print]
Babies born to mothers living near fracking operations are more likely to born prematurely, have low birth weight, and worse APGAR scores. Fracking chemicals are toxic to fetal development.
Shale gas development and infant health: Evidence from Pennsylvania.J Health Econ. 2018 Aug 13;61:134-150. doi: 10.1016/j.jhealeco.2018.07.004. [Epub ahead of print]
Infant mortality increases with air pollution. This study from Africa shows about the same relationship between infant mortality and air pollution, and adult mortality–a 1% increase for every 1 ug/m3 in PM2.5, or about 22% of infant deaths.
Heft-Neal S. et al. Robust relationship between air quality and infant mortality in AfricaNature volume 559, pages254–258 (2018)

Research Paper of the Month: Nov. 18, 2018
Research continues to build that air pollution is associated with a broad range of neurologic diseases. This study breaks new ground in finding a connection between air pollution and Amyotrophic Lateral Sclerosis (ALS), i.e. Lou Gehrig’s disease.
Povedano M, et al. Spatial Assessment of the Association between Long-Term Exposure to Environmental Factors and the Occurrence of Amyotrophic Lateral Sclerosis in Catalonia, Spain: A Population-Based Nested Case-Control Study. Neuroepidemiology. 2018 May 31;51(1-2):33-49. doi: 10.1159/000489664. [Epub ahead of print]
New and more detailed information about how air pollution damages the lungs. It actually causes a loss of the number of minute air sacs (alveoli) in the lungs when exposure occurs during prenatal or early post natal life.
Lopes dB, et al. Pre- and postnatal exposure of mice to concentrated urban PM2.5 decreases the number of alveoli and leads to altered lung function at an early stage of life. Environ Pollut. 2018 Jun 4;241:511-520. doi: 10.1016/j.envpol.2018.05.055. [Epub ahead of print]
More evidence that air pollution causes pregnancy complications like pre-term births, hypertension of pregnancy, and the most severe complications–miscarriage and still births.
Li X, et al. Analysis of short-term and sub-chronic effects of ambient air pollution on preterm birth in central China. Environ Sci Pollut Res Int. 2018 May 2. doi: 10.1007/s11356-018-2061-8. [Epub ahead of print]
Casey JA, et al. Coal and oil power plant retirements in California associated with reduced preterm birth among populations nearby. American Journal of Epidemiology, kwy110, https://doi.org/10.1093/aje/kwy110 Published: 16 May 2018
Xue T, et al. Association Between Hypertensive Disorders in Pregnancy and Particulate Matter in the Contiguous United States, 1999-2004. Hypertension. 2018 May 21. pii: HYPERTENSIONAHA.118.11080. doi: 10.1161/HYPERTENSIONAHA.118.11080. [Epub ahead of print].
Grippo A, et al. Air pollution exposure during pregnancy and spontaneous abortion and stillbirth. Rev Environ Health. 2018 Jul 5. pii: /j/reveh.ahead-of-print/reveh-2017-0033/reveh-2017-0033.xml. doi: 10.1515/reveh-2017-0033. [Epub ahead of print]
Another study showing that air pollution changes the chemical environment of placental DNA, increasing the vulnerability of the unborn to chronic disease later in life.
Maghbooli Z, et al. Air pollution during pregnancy and placental adaptation in the levels of global DNA methylation. PLoS One. 2018 Jul 6;13(7):e0199772. doi: 10.1371/journal.pone.0199772. eCollection 2018.
Another study showing that decreased pollution improved fertility rates.
Casey JA, et al. Increase in fertility following coal and oil power plant retirements in California. Environ Health. 2018 May 2;17(1):44. doi: 10.1186/s12940-018-0388-8.
We are learning more and more about how air pollution may contribute to inflammatory bowel diseases. This study in mice shows that air pollution disrupts the components of bowel bacteria, leaving the bowel more vulnerable to inflammation.
Mutlu EA, et al. Inhalational exposure to particulate matter air pollution alters the composition of the gut microbiome. Environ Pollut. 2018 May 18;240:817-830. doi: 10.1016/j.envpol.2018.04.130. [Epub ahead of print]
More epidemiologic evidence of air pollution increasing the risks for strokes and dementia
Béjot Y, et al. A review of epidemiological research on stroke and dementia and exposure to air pollution. Int J Stroke. 2018 Jan 1:1747493018772800. doi: 10.1177/1747493018772800. [Epub ahead of print]
Another study that suggests a connection between air pollution and brain cancer, and this one reveals a likely mechanism.
Ljubimova, JY, et al. Coarse particulate matter (PM2.5–10) in Los Angeles Basin air induces expression of inflammation and cancer biomarkers in rat brains. Scientific Reports, 2018; 8 (1) DOI: 10.1038/s41598-018-23885-3
This review article shows more evidence for the connection between air pollution and mental disorders, especially depression.
Buoli M, et al. Is there a link between air pollution and mental disorders?
Environ Int. 2018 Jun 4;118:154-168. doi: 10.1016/j.envint.2018.05.044. [Epub ahead of print]
More studies showing a significant connection between air pollution and suicide, substance abuse, and schizophrenia.
Lee H, et al. Ambient air pollution and completed suicide in 26 South Korean cities: Effect modification by demographic and socioeconomic factors. Sci Total Environ. 2018 Oct 15;639:944-951. doi: 10.1016/j.scitotenv.2018.05.210. Epub 2018 May 26.
Szyszkowicz M, et al. Ambient air pollution exposure and emergency department visits for substance abuse. PLoS One. 2018 Jun 29;13(6):e0199826. doi: 10.1371/journal.pone.0199826. eCollection 2018.
Duan J, et al. Is the serious ambient air pollution associated with increased admissions for schizophrenia? Sci Total Environ. 2018 Jul 2;644:14-19. doi: 10.1016/j.scitotenv.2018.06.218. [Epub ahead of print]
Another study showing that air pollution increases the incidence of infections in general, in this case, ear infections.
Park M, et al. Air pollution influences the incidence of otitis media in children: A national population-based study. PLoS One. 2018 Jun 28;13(6):e0199296. doi: 10.1371/journal.pone.0199296. eCollection 2018.
More evidence that air pollution impairs lung function in children.
Finke I, et al. Air pollution and airway resistance at age 8 years – the PIAMA birth cohort study. Environ Health. 2018 Jul 17;17(1):61. doi: 10.1186/s12940-018-0407-9.
We are often asked how bad does the air pollution have to get to make it more dangerous to your health than the benefits of the exercise itself? We still don’t really know the answer, but this study suggests that with dirty air, the benefits of the exercise are wiped out after 15 minutes, and that after 75 minutes, the air pollution is doing more damage than the benefits of the exercise.
Pasqua LA, et al. Exercising in Air Pollution: The Cleanest versus Dirtiest Cities Challenge.
Int J Environ Res Public Health. 2018 Jul 17;15(7). pii: E1502. doi: 10.3390/ijerph15071502.
This study suggests that breathing through tightly fitting N-95 masks reduces the amount of particles inhaled, but doesn’t decrease the body inflammation at the microscopic level, and therefore the health consequences of pollution.
More evidence that air pollution increases the risk of stomach cancer, and other cancers of the upper GI tract.
Nagel G, et al. Air pollution and incidence of cancers of the stomach and the upper aerodigestive tract in the European Study of Cohorts for Air Pollution Effects (ESCAPE). Int J Cancer. 2018 Apr 26. doi: 10.1002/ijc.31564. [Epub ahead of print]
Research Paper of the Month: April 27, 2018
We have become increasingly alarmed at the body of research showing how harmful air pollution is to the brain, including the presence of air pollution particles penetrating brain tissue itself.
The latest research examined the brains of 203 people, ranging in age from less than one year old to 40 years old. At autopsy (causes of death were usually trauma), every single brain but one showed the abnormal proteins that are the microbiologic hallmarks of Alzheimer’s, even in an 11 month old. And the amount of these abnormal proteins was proportional to the amount of air pollution where the subjects lived. The principle author, probably the world’s expert on this type of research said,
“Alzheimer’s disease hallmarks start in childhood in polluted environments, and we must implement effective preventative measures early. It is useless to take reactive actions decades later.”
Calderón-Garcidueñas L, et al. Hallmarks of Alzheimer disease are evolving relentlessly in Metropolitan Mexico City infants, children and young adults. APOE4 carriers have higher suicide risk and higher odds of reaching NFT stage V at ≤ 40 years of age. Environmental Research, 2018; 164: 475 DOI: 10.1016/j.envres.2018.03.023
This study was done evaluating a large patient population of over 100,000 right here on Utah’s Wasatch Front. It showed that serious lower respiratory infections in every age group, were increased with more air pollution, even short term exposure lasting only several days.
Horne BD, et al. Short-term Elevation of Fine Particulate Matter Air Pollution and Acute Lower Respiratory Infection. Am J Respir Crit Care Med. 2018 Apr 13. doi: 10.1164/rccm.201709-1883OC. [Epub ahead of print]
More evidence connecting air pollution to obesity, diabetes, and metabolic syndrome
Matthiessen C, et al. Long-term exposure to airborne particulate matter and NO2 and prevalent and incident metabolic syndrome – Results from the Heinz Nixdorf Recall Study. Environ Int. 2018 Apr 10;116:74-82. doi: 10.1016/j.envint.2018.02.035. [Epub ahead of print]
Yang BY, et al. Ambient air pollution in relation to diabetes and glucose-homoeostasis markers in China: a cross-sectional study with findings from the 33 Communities Chinese Health Study. Lancet Planet Health. 2018 Feb;2(2):e64-e73. doi: 10.1016/S2542-5196(18)30001-9. Epub 2018 Feb 9.
Lucht SA, et al. Air Pollution and Glucose Metabolism: An Analysis in Non-Diabetic Participants of the Heinz Nixdorf Recall Study. Environ Health Perspect. 2018 Apr 3;126(4):047001. doi: 10.1289/EHP2561.
Wang M, et al. Association between Short-Term Exposure to Air Pollution and Dyslipidemias among Type 2 Diabetic Patients in Northwest China: A Population-Based Study. Int J Environ Res Public Health. 2018 Mar 30;15(4). pii: E631. doi: 10.3390/ijerph15040631.
This study demonstrated with one mechanism of air pollution’s effect on the lungs is the triggering of cell death in the lining of the airways.
Xu F, et al. Necroptosis Contributes to Urban Particulate Matter-Induced Airway Epithelial Injury. Cell Physiol Biochem. 2018 Mar 29;46(2):699-712. doi: 10.1159/000488726. [Epub ahead of print]
More evidence that air pollution changes the functioning of genes, one mechanism by which it provokes diseases of the heart, lungs, and endocrine systems.
Favé M-J, et al. Gene-by-environment interactions in urban populations modulate risk phenotypes. Nature Communications, 2018; 9 (1) DOI: 10.1038/s41467-018-03202-2
Plusquin M, et al. DNA methylome marks of exposure to particulate matter at three time points in early life. Environ Sci Technol. 2018 Mar 30. doi: 10.1021/acs.est.7b06447. [Epub ahead of print]
Jie Y, et al. Changes in gene expression in lungs of mice exposed to traffic-related air pollution. Mol Cell Probes. 2018 Apr 2. pii: S0890-8508(18)30034-3. doi: 10.1016/j.mcp.2018.03.005. [Epub ahead of print].
Domingues ÉP, et al. Genotoxic effects following exposure to air pollution in street vendors from a high-traffic urban area. Environ Monit Assess. 2018 Mar 14;190(4):215. doi: 10.1007/s10661-018-6598-2.
Krauskopf J, Caiment F, van Veldhoven K, Chadeau-Hyam M, Sinharay R, Chung KF, Cullinan P, Collins P, Barratt B, Kelly FJ, Vermeulen R, Vineis P, de Kok TM, Kleinjans JC. The human circulating miRNome reflects multiple organ disease risks in association with short-term exposure to traffic-related air pollution. Environ Int. 2018 Jan 27;113:26-34. doi: 10.1016/j.envint.2018.01.014. [Epub ahead of print] PMID: 29421404 [PubMed – as supplied by publisher]
More evidence connecting air pollution to autism
Kalkbrenner A, et al. Air Toxics in Relation to Autism Diagnosis, Phenotype, and Severity in a U.S. Family-Based Study. Environ Health Perspect; DOI:10.1289/EHP1867
People living near oil and gas drilling operations have a higher incidence of preterm birth.
Whitworth KW, et al. Drilling and Production Activity Related to Unconventional Gas Development and Severity of Preterm Birth. Environ Health Perspect; DOI:10.1289/EHP2622
Lead is usually thought of only as a neurotoxin, with focus primarily on what it does to the brain development of children. But lead exposure is also associated with a higher mortality rate among adults, contributing to over 400,000 deaths a year from heart disease.
Lanphear B, et al. Low-level lead exposure and mortality in US adults: a population-based cohort study. The Lancet Public Health, 2018 DOI: 10.1016/S2468-2667(18)30025-2
More evidence that air pollution contributes to the risk of strokes
Kulick ER, et al. Residential Proximity to Major Roadways and Risk of Incident Ischemic Stroke in NOMAS (The Northern Manhattan Study). Stroke. 2018 Mar 14. pii: STROKEAHA.117.019580. doi: 10.1161/STROKEAHA.117.019580. [Epub ahead of print]
Black Americans suffer higher cardiovascular risk from air pollution than do caucasians.
Erqou S, et al. Particulate Matter Air Pollution and Racial Differences in Cardiovascular Disease Risk. Arterioscler Thromb Vasc Biol. 2018 Mar 15. pii: ATVBAHA.117.310305. doi: 10.1161/ATVBAHA.117.310305. [Epub ahead of print]
More evidence that air pollution causes an increase risk for the pregnancy complication known as preeclampsia.
Wang Q, et al. Effects of prenatal exposure to air pollution on preeclampsia in Shenzhen, China. Environ Pollut. 2018 Feb 18;237:18-27. doi: 10.1016/j.envpol.2018.02.010. [Epub ahead of print]
More air pollution exposure is associated with smaller volumes of brain grey matter.
Power MC, et al. The Association of Long-Term Exposure to Particulate Matter Air Pollution with Brain MRI Findings: The ARIC Study. Environ Health Perspect. 2018 Feb 16;126(2):027009. doi: 10.1289/EHP2152.
This is another study showing increased risk for congenital heart defects with more air pollution.
Ren Z, et al. Maternal exposure to ambient PM10 during pregnancy increases the risk of congenital heart defects: Evidence from machine learning models. Sci Total Environ. 2018 Feb 19;630:1-10. doi: 10.1016/j.scitotenv.2018.02.181. [Epub ahead of print]
More evidence that air pollution increases blood pressure and arterial stiffness, and one of these studies showed that radioactive pollution particles also increased blood pressure.
Baumgartner J, et al. Household air pollution and measures of blood pressure, arterial stiffness and central haemodynamics. Heart. 2018 Feb 9. pii: heartjnl-2017-312595. doi: 10.1136/heartjnl-2017-312595. [Epub ahead of print]
Nyhan MM, et al. Associations Between Ambient Particle Radioactivity and Blood Pressure: The NAS (Normative Aging Study). J Am Heart Assoc. 2018 Mar 15;7(6). pii: e008245. doi: 10.1161/JAHA.117.008245.
Salameh P, et al. Hypertension prevalence and living conditions related to air pollution: results of a national epidemiological study in Lebanon. Environ Sci Pollut Res Int. 2018 Feb 13. doi: 10.1007/s11356-018-1411-x. [Epub ahead of print]
Some of the increased risk for heart attack maybe related to the rate of rise in air pollution. In other words, a rapid rise in pollution may have more of an impact than the eventual pollution concentration itself.
Rasche M, et al. Rapid increases in nitrogen oxides are associated with acute myocardial infarction: A case-crossover study. Eur J Prev Cardiol. 2018 Jan 1:2047487318755804. doi: 10.1177/2047487318755804. [Epub ahead of print]
Air pollution causes increased fragmentation of human sperm.
Bosco L, et al. Sperm DNA fragmentation: An early and reliable marker of air pollution.
Environ Toxicol Pharmacol. 2018 Feb 7;58:243-249. doi: 10.1016/j.etap.2018.02.001. [Epub ahead of print]
Here’s one we wouldn’t have thought of. We know air pollution affects brain function, including increasing depression, suicidal tendencies, and impairing cognition. This study shows that air pollution is associated with criminal activity and unethical behavior.
Lu J, et al. Polluted Morality: Air Pollution Predicts Criminal Activity and Unethical Behavior. Psychological Science, 2018; 095679761773580 DOI: 10.1177/0956797617735807
Air pollution exposure during pregnancy increases the risk of asthma after birth during childhood.
Lavigne É, Bélair MA, Rodriguez Duque D, Do MT, Stieb DM, Hystad P, van Donkelaar A, Martin RV, Crouse DL, Crighton E, Chen H, Burnett RT, Weichenthal S, Villeneuve PJ, To T, Brook JR, Johnson M, Cakmak S, Yasseen AS 3rd, Walker M. Effect modification of perinatal exposure to air pollution and childhood asthma incidence. Eur Respir J. 2018 Feb 1. pii: 1701884. doi: 10.1183/13993003.01884-2017.
Another study showing increased rates of death with short term air pollution.
Huang J, Pan X, Guo X, Li G. Impacts of air pollution wave on years of life lost: A crucial way to communicate the health risks of air pollution to the public. Environ Int. 2018 Jan 29;113:42-49. doi: 10.1016/j.envint.2018.01.022. [Epub ahead of print] PMID: 29421406 [PubMed – as supplied by publisher]
The association between air pollution and still births continue to mount.
Yang S, Tan Y, Mei H, Wang F, Li N, Zhao J, Zhang Y, Qian Z, Chang JJ, Syberg KM, Peng A, Mei H, Zhang D, Zhang Y, Xu S, Li Y, Zheng T, Zhang B. Ambient air pollution the risk of stillbirth: A prospective birth cohort study in Wuhan, China. Int J Hyg Environ Health. 2018 Feb 5. pii: S1438-4639(17)30531-X. doi: 10.1016/j.ijheh.2018.01.014. [Epub ahead of print] PMID: 29422441 [PubMed – as supplied by publisher]
Air pollution is associated relapses in multiple sclerosis
Jeanjean M, Bind MA, Roux J, Ongagna JC, de Sèze J, Bard D, Leray E. Ozone, NO<sub>2</sub> and PM<sub>10</sub> are associated with the occurrence of multiple sclerosis relapses. Evidence from seasonal multi-pollutant analyses. Environ Res. 2018 Feb 6;163:43-52. doi: 10.1016/j.envres.2018.01.040. [Epub ahead of print] PMID: 29426027 [PubMed – as supplied by publisher]
Chronic Obstructive Pulmonary Disease (COPD) is usually thought of as a disease related to smoking. But it is also related to air pollution exposure.
Lin H, Qian ZM, Guo Y, Zheng Y, Ai S, Hang J, Wang X, Zhang L, Liu T, Guan W, Li X, Xiao J, Zeng W, Xian H, Howard SW, Ma W, Wu F. The attributable risk of chronic obstructive pulmonary disease due to ambient fine particulate pollution among older adults. Environ Int. 2018 Feb 5;113:143-148. doi: 10.1016/j.envint.2018.01.029. [Epub ahead of print] PMID: 29425898 [PubMed – as supplied by publisher]
The American Thoracic Society has recommended lower national air quality standards than currently established by the EPA. The ATS recommend a PM2.5 standard of 11 ug/m3 instead of 12, and an ozone standard of 60 ppm instead of 70. This study calculates the increased mortality resulting from air pollution above the ATS suggestions.
Cromar KR, Gladson LA, Ghazipura M, Ewart G. ATS and Marron Institute Report: Estimated Excess Morbidity and Mortality Associated with Air Pollution above ATS-Recommended Standards, 2013-2015. Ann Am Thorac Soc. 2018 Feb 9. doi: 10.1513/AnnalsATS.201710-785EH. [Epub ahead of print] No abstract available.
PMID: 29425050 [PubMed – as supplied by publisher]
Air pollution increases atherosclerosis in arteries in the brain and ameliorated by consuming omega three fatty acids.
Guan L, et al. PM2.5 inhalation induces intracranial atherosclerosis which may be ameliorated by omega 3 fatty acids. Oncotarget. 2017 Dec 16;9(3):3765-3778. doi: 10.18632/oncotarget.23347. eCollection 2018 Jan 9.
Research Paper of the Month: Jan. 27, 2018
We highlight this paper first because one of our board members, Dr. Robert Paine, was one of the authors and the study was done here on the Wasatch Front. Investigators from the University of Utah and Intermountain Medical Center found that the risk of pneumonia and the severity of the illness (including ICU admission and need for critical care) was increased in response to a few days of increased PM2.5 levels. Like with so many other studies, these effects were seen even at levels below EPA standards.
Pirozzi CS, Jones BE, VanDerslice JA, Zhang Y, Paine R, Dean N. Short-Term Air Pollution and Incident Pneumonia: A Case-Crossover Study. Ann Am Thorac Soc. 2017 Dec 28. doi: 10.1513/AnnalsATS.201706-495OC. [Epub ahead of print]
More research showing the relationship between air pollution and adverse birth outcomes. In the case of the study below, an analysis of over 1.3 million births in China showed not only higher rates of pre-term births with more air pollution, but the correlation was stronger the more premature the birth.
Wang YY, et al. Association of Long-term Exposure to Airborne Particulate Matter of 1 μm or Less With Preterm Birth in China. JAMA Pediatr. 2018 Jan 2:e174872. doi: 10.1001/jamapediatrics.2017.4872. [Epub ahead of print]
Air pollution exposure during the first trimester was associated with decreased weight of a pregnant mother’s placenta.
Ghasemi-Tehrani H, et al. Effect of Exposure to Air Pollution on Placental Weight in Isfahan-Iran. J Family Reprod Health. 2017 Jun;11(2):90-96.
Shutting down a coal power plant was followed by an increase in birth weight of newborns downwind from the plant.
Yang M, et al. The Impact of Environmental Regulation on Fetal Health: Evidence from the Shutdown of a Coal-Fired Power Plant Located Upwind of New Jersey. Journal of Environmental Economics and Management, 2017; DOI: 10.1016/j.jeem.2017.11.005
More evidence of air pollution contributes to metabolic disorders, i.e. type II diabetes, insulin resistance, and interferes with glucose metabolism.
Chen M, et al. Prenatal Exposure to Diesel Exhaust PM2.5 Causes Offspring β Cell Dysfunction in Adulthood.
Am J Physiol Endocrinol Metab. 2017 Dec 26. doi: 10.1152/ajpendo.00336.2017. [Epub ahead of print]
Khafaie MA, et al. Particulate matter and markers of glycemic control and insulin resistance in type 2 diabetic patients: result from Wellcome Trust Genetic study. J Expo Sci Environ Epidemiol. 2017 Dec 21. doi: 10.1038/s41370-017-0001-1. [Epub ahead of print]
Dendup T, et al. Environmental Risk Factors for Developing Type 2 Diabetes Mellitus: A Systematic Review.
Int J Environ Res Public Health. 2018 Jan 5;15(1). pii: E78. doi: 10.3390/ijerph15010078.
Bai L, et al. Exposure to Ambient Ultrafine Particles and Nitrogen Dioxide and Incident Hypertension and Diabetes.
Epidemiology. 2018 Jan 9. doi: 10.1097/EDE.0000000000000798. [Epub ahead of print]
Tan C, et al. Long-term high air pollution exposure induced metabolic adaptations in traffic policemen.
Environ Toxicol Pharmacol. 2018 Jan 5;58:156-162. doi: 10.1016/j.etap.2018.01.002. [Epub ahead of print]
More studies showing air pollution, including ozone, increases blood pressure, and the risk for hospitalization for high blood pressure
Zhang Z, et al. Long-Term Exposure to Fine Particulate Matter, Blood Pressure, and Incident Hypertension in Taiwanese Adults. Environ Health Perspect. 2018 Jan 18;126(1):017008. doi: 10.1289/EHP2466.
Chen CC, et al. Association between gaseous air pollution and hospital admissions for hypertension in Taipei, Taiwan.
J Toxicol Environ Health A. 2017 Dec 22:1-7. doi: 10.1080/15287394.2017.1395573. [Epub ahead of print]
Two researcher papers showing that air pollution is associated with aggravation of heart failure.
Buteau S, et al. Associations between ambient air pollution and daily mortality in a cohort of congestive heart failure: Case-crossover and nested case-control analyses using a distributed lag nonlinear model. Environ Int. 2018 Jan 17. pii: S0160-4120(17)31563-5. doi: 10.1016/j.envint.2018.01.003. [Epub ahead of print]
Ji X, et al. Potential Role of Inflammation in Associations between Particulate Matter and Heart Failure. Curr Pharm Des. 2018 Jan 10. doi: 10.2174/1381612824666180110150550. [Epub ahead of print]
This study shows that air pollution is associated with increasing calcification of heart valves.
Tibuakuu M, et al. Exposure to ambient air pollution and calcification of the mitral annulus and aortic valve: the multi-ethnic study of atherosclerosis (MESA). Environ Health. 2017 Dec 21;16(1):133. doi: 10.1186/s12940-017-0346-x.
Air pollution is associated with higher risk for developing and seeking treatment for mental disorders, and a much higher mortality risk for those with mental health and behavioral disorders, including suicide.
Ho HC, et al. Spatiotemporal influence of temperature, air quality, and urban environment on cause-specific mortality during hazy days. Environment International, Volume 112, March 2018, Pages 10-22
Jia Z, et al. Exposure to Ambient Air Particles Increases the Risk of Mental Disorder: Findings from a Natural Experiment in Beijing. Int J Environ Res Public Health. 2018 Jan 19;15(1). pii: E160. doi: 10.3390/ijerph15010160.
Oudin A, et al. The association between daily concentrations of air pollution and visits to a psychiatric emergency unit: a case-crossover study.Environ Health. 2018 Jan 10;17(1):4. doi: 10.1186/s12940-017-0348-8.Casas L, et al. Does air pollution trigger suicide? A case-crossover analysis of suicide deaths over the life span
European Journal of Epidemiology. November 2017, Volume 32, Issue 11, pp 973–981
A good review article on how environmental contaminates like air pollution affect the brain in males much more than females
Kern JK, et al. Developmental neurotoxicants and the vulnerable male brain: a systematic review of suspected neurotoxicants that disproportionally affect males. Acta Neurobiol Exp (Wars). 2017;77(4):269-296.
More evidence of air pollution increasing a person’s risk for stroke.
Guan T, et al. Differential Susceptibility in Ambient Particle-Related First-Ever Stroke Onset Risk: Findings From a National Case-Crossover Study. Am J Epidemiol. 2018 Jan 17. doi: 10.1093/aje/kwy007. [Epub ahead of print]
This study showed that a biological pathway for air pollution’s involvement in strokes and heart attacks is the release of inflammatory chemicals that alter the functioning of genes involved in the regulation of blood vessels.
Chen R, et al. Fine Particulate Air Pollution and the Expression of microRNAs and Circulating Cytokines Relevant to Inflammation, Coagulation, and Vasoconstriction. Environ Health Perspect. 2018 Jan 17;126(1):017007. doi: 10.1289/EHP1447.
This study in mice shows that an anti-oxidant in grapefruit, reduces the DNA damage and oxidative stress in heart cells, and the tendency for blood clot formation caused by diesel exhaust. This is just one study, but there’s no down side to eating more grapefruit.
Nemmar A, et al. Thrombosis, systemic and cardiac oxidative stress and DNA damage induced by pulmonary exposure to diesel exhaust particles, and the effect of nootkatone thereon. Am J Physiol Heart Circ Physiol. 2018 Jan 5. doi: 10.1152/ajpheart.00313.2017. [Epub ahead of print]
Multiple studies have shown air pollution affects male sperm. The studies below add to that data base, including one that shows it reduces the y/x chromosome ratio in sperm which would result in a decrease in percentage of male newborns compared to females.
Radwan M, et al. Air Pollution and Human Sperm Sex Ratio. Am J Mens Health. 2018 Jan 1:1557988317752608. doi: 10.1177/1557988317752608. [Epub ahead of print]
Zhou N, et al. Exposures to Atmospheric PM10 and PM10-2.5 Affect Male Semen Quality: Results of MARHCS Study.
Environ Sci Technol. 2018 Jan 11. doi: 10.1021/acs.est.7b05206. [Epub ahead of print]
This is the first study we know of to show that air pollution affects menstruation, delaying the onset of menstrual regularity in exposed teenage girls.
Mahalingaiah S, et al. Perimenarchal air pollution exposure and menstrual disorders. Human Reproduction, 2018; DOI: 10.1093/humrep/dey005
Air pollution even of only a few days duration, increases the risk of bronchiolitis and otitis media in infants, especially those born prematurely
Girguis MS, et al. Exposure to acute air pollution and risk of bronchiolitis and otitis media for preterm and term infants.
J Expo Sci Environ Epidemiol. 2017 Dec 21. doi: 10.1038/s41370-017-0006-9. [Epub ahead of print]
Research Paper of the Month: Dec. 19, 2017
Hundreds of studies have shown increased overall mortality from air pollution, most of that is assumed to occur in the vulnerable subsets of the adult population, especially the elderly. Far fewer studies have been done exploring possible increased rates of infant mortality. The study below adds significantly to the evidence that air pollution also contributes to infant mortality. Almost 500,000 infants were tracked for over 6 years. Researchers found a very strong association between small increases in PM2.5 and total infant deaths, respiratory deaths, and SIDS. Specifically 1.3 ug/m3 increases in PM2.5 increased the rate of these outcomes between 200% and 300%.
Son JY, et al. Pregnancy and Lifetime Exposure to Fine Particulate Matter and Infant Mortality in Massachusetts, 2001-2007. Am J Epidemiol. 2017 Nov 7:1-9. doi: 10.1093/aje/kwx015. [Epub ahead of print]
Acceleration of the aging process is part of the clinical consequence of air pollution exposure. Telomere length is a marker of biological aging. This study showed that prenatal air pollution provokes shorter telomere length in the newborns, measured in the umbilical cord and placenta.
Martens DS, et al. Prenatal Air Pollution and Newborns’ Predisposition to Accelerated Biological Aging.
JAMA Pediatr. 2017 Oct 16. doi: 10.1001/jamapediatrics.2017.3024. [Epub ahead of print]
More evidence that air pollution triggers lung cancer.
Lamichhane DK, et al. Lung Cancer Risk and Residential Exposure to Air Pollution: A Korean Population-Based Case-Control Study. Yonsei Med J. 2017 Nov;58(6):1111-1118. doi: 10.3349/ymj.2017.58.6.1111.
Air pollution and a more deprived social environment both contribute to lower intellectual scores in children.
Lett LA, et al. The Combined Influence of Air Pollution and Home Learning Environment on Early Cognitive Skills in Children. Int J Environ Res Public Health. 2017 Oct 26;14(11). pii: E1295. doi: 10.3390/ijerph14111295.
Given that inflammation is the biological pathway through which air pollution causes many diseases, for this study to find an exacerbation of lupus with air pollution is not at all surprising.
Alves AGF, et al. Influence of air pollution on airway inflammation and disease activity in childhood-systemic lupus erythematosus. Clin Rheumatol. 2017 Nov 2. doi: 10.1007/s10067-017-3893-1. [Epub ahead of print]
Numerous new studies showing air pollution’s association with adverse pregnancy outcomes, especially low birth weight syndrome.
Wu H, et al. Exposure to fine particulate matter during pregnancy and risk of term low birth weight in Jinan, China, 2014-2016.
Int J Hyg Environ Health. 2017 Oct 28. pii: S1438-4639(17)30399-1. doi: 10.1016/j.ijheh.2017.10.013. [Epub ahead of print]
Ji Y, et al. Association between exposure to particulate matter during pregnancy and birthweight: a systematic review and a meta-analysis of birth cohort studies. J Biomed Res. 2017 Nov 1. doi: 10.7555/JBR.31.20170038. [Epub ahead of print]
Dutta A, et al. Household air pollution and chronic hypoxia in the placenta of pregnant Nigerian women: A randomized controlled ethanol Cookstove intervention. Sci Total Environ. 2017 Nov 14;619-620:212-220. doi: 10.1016/j.scitotenv.2017.11.091. [Epub ahead of print]
Smith R, et al. Impact of London’s road traffic air and noise pollution on birth weight: retrospective population based cohort study. BMJ, 2017; j5299 DOI: 10.1136/bmj.j5299
Air pollution exposure of a mother, measured one month prior to conception and one month after shows higher rates of congenital malformations, especially of the heart.
Ren S, et al. Periconception Exposure to Air Pollution and Risk of Congenital Malformations. The Journal of Pediatrics, 2017; DOI: 10.1016/j.jpeds.2017.09.076
Air pollution affects the brain in multiple ways. This shows that it increases the delinquent behavior of adolescents, much like lead does.
Younan D, et al. Longitudinal Analysis of Particulate Air Pollutants and Adolescent Delinquent Behavior in Southern California. Journal of Abnormal Child Psychology, 2017; DOI: 10.1007/s10802-017-0367-5
This study shows that attention span in school children is impaired by the air pollution they breathed on the way to school.
Sunyer J, et al. Traffic-related Air Pollution and Attention in Primary School Children: Short-term Association. Epidemiology: March 2017 – Volume 28 – Issue 2 – p 181–189. doi: 10.1097/EDE.0000000000000603
Two more studies that show a connection between air pollution and autism. The first study showed that the affect could be mitigated by maternal extra consumption of folic acid.
Goodrich AJ, et al. Joint effects of prenatal air pollutant exposure and maternal folic acid supplementation on risk of autism spectrum disorder. Autism Res. 2017 Nov 9. doi: 10.1002/aur.1885. [Epub ahead of print]
Li K, et al. Early postnatal exposure to airborne fine particulate matter induces autism-like phenotypes in male rats. Toxicol Sci. 2017 Nov 7. doi: 10.1093/toxsci/kfx240. [Epub ahead of print]
Evidence for a mechanism of how prenatal air pollution exposure may be associated with increased risk of childhood obesity.
Alderete TL, et al. Prenatal traffic-related air pollution exposures, cord blood adipokines and infant weight. Pediatr Obes. 2017 Nov 3. doi: 10.1111/ijpo.12248. [Epub ahead of print]
This is first study we know of to show that osteoporosis is associated with air pollution exposure.
Prada, D, Zhong, J, Colicino, E et al. Association of air particulate pollution with bone loss over time and bone fracture risk: analysis of data from two independent studies. Lancet Planet Health. 2017; 1: e337–e347
Air pollution degrades the inside lining of the nose.
Zhao R, et al. Nasal epithelial barrier disruption by particulate matter ≤2.5 μm via tight junction protein degradation.
J Appl Toxicol. 2017 Dec 13. doi: 10.1002/jat.3573. [Epub ahead of print]
Biomass smoke (like wood) causes DNA damage in cell death in the lung.
de Oliveira Alves N, et al. Biomass burning in the Amazon region causes DNA damage and cell death in human lung cells. Scientific Reports, 2017; 7 (1) DOI: 10.1038/s41598-017-11024-3
Numerous new studies on the association between air pollution and premature death.
Kim SE, et al. Associations between mortality and prolonged exposure to elevated particulate matter concentrations in East Asia. Environ Int. 2017 Oct 30. pii: S0160-4120(17)30909-1. doi: 10.1016/j.envint.2017.10.010. [Epub ahead of print]
Fang X, et al. Relationship between fine particulate matter, weather condition and daily non-accidental mortality in Shanghai, China: A Bayesian approach. PLoS One. 2017 Nov 9;12(11):e0187933. doi: 10.1371/journal.pone.0187933. eCollection 2017.
Holnicki P, et al. Burden of Mortality and Disease Attributable to Multiple Air Pollutants in Warsaw, Poland. Int J Environ Res Public Health. 2017 Nov 8;14(11). pii: E1359. doi: 10.3390/ijerph14111359.
Cappellari M, et al. Association between short- and medium-term air pollution exposure and risk of mortality after intravenous thrombolysis for stroke. J Thromb Thrombolysis. 2017 Nov 28. doi: 10.1007/s11239-017-1589-7. [Epub ahead of print]
Corrigan AE, et al. Fine particulate matters: The impact of air quality standards on cardiovascular mortality. Environ Res. 2017 Nov 28;161:364-369. doi: 10.1016/j.envres.2017.11.025. [Epub ahead of print]
Parker JD, et al. Particulate Matter Air Pollution Exposure and Heart Disease Mortality Risks by Race and Ethnicity in the United States: 1997-2009 NHIS with Mortality Followup Through 2011. Circulation. 2017 Dec 13. pii: CIRCULATIONAHA.117.029376. doi: 10.1161/CIRCULATIONAHA.117.029376. [Epub ahead of print]
In this rather elaborate study, the heart and lung benefits of exercise walking were offset by air pollution inhaled along a busy road.
Sinharay R, et al. Respiratory and cardiovascular responses to walking down a traffic-polluted road compared with walking in a traffic-free area in participants aged 60 years and older with chronic lung or heart disease and age-matched healthy controls: a randomised, crosso. The Lancet, 2017; DOI:
More evidence that air pollution increases blood pressure
Magalhaes S, et al. Impacts of exposure to black carbon, elemental carbon, and ultrafine particles from indoor and outdoor sources on blood pressure in adults: A review of epidemiological evidence. Environ Res. 2017 Nov 28;161:345-353. doi: 10.1016/j.envres.2017.11.030. [Epub ahead of print]
This study in animals shows impaired sperm production with air pollution exposure
Qiu L, et al. Exposure to Concentrated Ambient PM2.5 Compromises Spermatogenesis in a Mouse Model: Role of Suppression of Hypothalamus-Pituitary-Gonads Axis. Toxicol Sci. 2017 Nov 20. doi: 10.1093/toxsci/kfx261. [Epub ahead of print]
Research Paper of the Month: Oct. 16, 2017
We have stated previously that air pollution harms all major organ systems. The evidence for an affect on kidneys has been sparse however. This new study shows evidence that air pollution has a significant association with impaired kidney function.
Bowe B, et al. Particulate Matter Air Pollution and the Risk of Incident CKD and Progression to ESRD. J Am Soc Nephrol. 2017 Sep 21. pii: ASN.2017030253. doi: 10.1681/ASN.2017030253. [Epub ahead of print]
Another study showing air pollution’s connection to rates of strokes.
Guo P, et al. Ambient Air Pollution and Risk for Ischemic Stroke: A Short-Term Exposure Assessment in South China. Int J Environ Res Public Health. 2017 Sep 20;14(9). pii: E1091. doi: 10.3390/ijerph14091091.
More evidence of the harm that air pollution provokes on fetal development, placental growth and pregnancy outcomes.
Blum J, et al. Exposure to Ambient Particulate Matter during Specific Gestational Periods Produces Adverse Obstetric Consequences in Mice. Environmental Health Perspectives, July 2017 DOI: 10.1289/EHP1029
Soto SF, et al. Exposure to fine particulate matter in the air alters placental structure and the renin-angiotensin system. PLoS One. 2017 Aug 18;12(8):e0183314. doi: 10.1371/journal.pone.0183314. eCollection 2017.
Reis MMD, et al. Air pollution and low birth weight in an industrialized city in Southeastern Brazil, 2003-2006. Rev Bras Epidemiol. 2017 Apr-Jun;20(2):189-199. doi: 10.1590/1980-5497201700020001.
Clemens T, et al. Maternal exposure to ambient air pollution and fetal growth in North-East Scotland: A population-based study using routine ultrasound scans. Environ Int. 2017 Oct;107:216-226. doi: 10.1016/j.envint.2017.07.018. Epub 2017 Jul 25.
Kingsley SL, et al. Maternal residential air pollution and placental imprinted gene expression. Environ Int. 2017 Sep 5;108:204-211. doi: 10.1016/j.envint.2017.08.022. [Epub ahead of print]
Wang L, et al. The association between cooking oil fume exposure during pregnancy and birth weight: A prospective mother-child cohort study. Sci Total Environ. 2017 Sep 4;612:822-830. doi: 10.1016/j.scitotenv.2017.08.031. [Epub ahead of print]
Air pollution is associated with brain diseases and dysfunction. This study adds to the evidence that air pollution contributes to depression.
Lin H, et al. Exposure to air pollution and tobacco smoking and their combined effects on depression in six low- and middle-income countries. Br J Psychiatry. 2017 Aug 10. pii: bjp.bp.117.202325. doi: 10.1192/bjp.bp.117.202325. [Epub ahead of print]
Another study showing that air pollution impairs cognitive abilities of children. In particular these studies measured the amount of air pollution that children breathed on the way to school, which correlated with decreased memory.
Forns J, et al. Longitudinal association between air pollution exposure at school and cognitive development in school children over a period of 3.5 years. Environ Res. 2017 Aug 28;159:416-421. doi: 10.1016/j.envres.2017.08.031. [Epub ahead of print]
Alvarez-Pedrerol M, et al. Impact of commuting exposure to traffic-related air pollution on cognitive development in children walking to school. Environmental Pollution, 2017; 231: 837 DOI: 10.1016/j.envpol.2017.08.075
More studies showing air pollution’s strong association with Alzheimer’s, dementia, and the anatomic changes in the brain associated with these disorders
Hullmann M, et al. Diesel engine exhaust accelerates plaque formation in a mouse model of Alzheimer’s disease. Part Fibre Toxicol. 2017 Aug 30;14(1):35. doi: 10.1186/s12989-017-0213-5.
Chen H, et al. Exposure to ambient air pollution and the incidence of dementia: A population-based cohort study. Environment International. Volume 108, November 2017, Pages 271-277
Another study showing air pollution’s connection to premature death, in this case due to cardiovascular disease, and more pronounced in women.
Zhang C, et al. Association between air pollution and cardiovascular mortality in Hefei, China: A time-series analysis. Environ Pollut. 2017 Aug 7. pii: S0269-7491(16)32799-3. doi: 10.1016/j.envpol.2017.06.022. [Epub ahead of print]
Benzene, SO2, and NOx were associated with increased rates of lung and bladder cancer, primarily in women over the age of 75.
Collarile P, et al. Residence in Proximity of a Coal-Oil-Fired Thermal Power Plant and Risk of Lung and Bladder Cancer in North-Eastern Italy. A Population-Based Study: 1995-2009.
In utero exposure to air pollution, specifically diesel exhaust, has been shown in animals to lead to heart failure in adulthood. This study showed that a likely mechanism is the alteration of genes that play a role in the the functioning of heart cells.
Goodson J, et al. In utero exposure to diesel exhaust particulates is associated with an altered cardiac transcriptional response to transverse aortic constriction and altered DNA methylation. The FASEB Journal, 2017; fj.201700032R DOI: 10.1096/fj.201700032R
This study shows that in healthy college age students, higher air pollution led to significant increases in stress hormones–cortisol, cortisone, epinephrine, and norepinephrine, higher blood pressure, insulin resistance, and biomarkers of oxidative stress and inflammation
Li H, et al. Particulate Matter Exposure and Stress Hormone Levels: A Randomized, Double-Blind, Crossover Trial of Air Purification. https://doi.org/10.1161/CIRCULATIONAHA.116.026796 Circulation. 2017;136:618-627
More studies that strengthen the connection between air pollution and type II diabetes.
Mazidi M, et al. Ambient particulate air pollution (PM2.5) is associated with the ratio of type 2 diabetes to obesity. Sci Rep. 2017 Aug 22;7(1):9144. doi: 10.1038/s41598-017-08287-1.
Strak M, et al. Long-term exposure to particulate matter, NO2 and the oxidative potential of particulates and diabetes prevalence in a large national health survey. Environ Int. 2017 Sep 5;108:228-236. doi: 10.1016/j.envint.2017.08.017. [Epub ahead of print]
More studies showing particulate pollution’s alteration of the functioning of genes.
Huang Q, et al. Fine particulate matter 2.5 exerted its toxicological effect by regulating a new layer, long non-coding RNA. Sci Rep. 2017 Aug 24;7(1):9392. doi: 10.1038/s41598-017-09818-6.
de Oliveira A, et al. Biomass burning in the Amazon region causes DNA damage and cell death in human lung cells. Sci Rep. 2017 Sep 7;7(1):10937. doi: 10.1038/s41598-017-11024-3.
More evidence that air pollution shortens life expectancy and causes premature death.
Ebenstein A, et al. New evidence on the impact of sustained exposure to air pollution on life expectancy from China’s Huai River Policy. Proceedings of the National Academy of Sciences, 2017; 201616784 DOI: 10.1073/pnas.1616784114
Huang C, et al. Potential Cardiovascular and Total Mortality Benefits of Air Pollution Control in Urban China. Circulation. 2017 Sep 7. pii: CIRCULATIONAHA.116.026487. doi: 10.1161/CIRCULATIONAHA.116.026487. [Epub ahead of print.
Malley C, et al. Updated Global Estimates of Respiratory Mortality in Adults ≥30 Years of Age Attributable to Long-Term Ozone Exposure. Environ Health Perspect; DOI:10.1289/EHP1390
Blount, R, et al. Traffic-Related Air Pollution and All-Cause Mortality during Tuberculosis Treatment in California. Environ Health Perspect; DOI:10.1289/EHP1699
Inhalation of particles is different depending on the age of the person. Particle deposition highest in an infant, less in an older child, and lowest in an adult.
Deng Q, et al. Particle deposition in tracheobronchial airways of an infant, child and adult. Sci Total Environ. 2017 Aug 27;612:339-346. doi: 10.1016/j.scitotenv.2017.08.240. [Epub ahead of print]
Another study that shows a connection between air pollution and malignant brain tumors
Andersen Z, et al. Long-term Exposure to Ambient Air Pollution and Incidence of Brain Tumor: the European Study of Cohorts for Air Pollution Effects (ESCAPE). Neuro Oncol. 2017 Aug 31. doi: 10.1093/neuonc/nox163. [Epub ahead of print]
More evidence that air pollution is associated with increased susceptibility to heart failure
Sørensen M, et al. Long-Term Exposure to Road Traffic Noise and Nitrogen Dioxide and Risk of Heart Failure: A Cohort Study. Environ Health Perspect. 2017 Sep 26;125(9):097021. doi: 10.1289/EHP1272.
Epigenetic changes has been found to play a role in the inflammation cascade triggered by air pollution.
Wang C, et al. Acute Inflammation Following Personal Exposure to Fine-particulate Air Pollution. Am J Epidemiol. 2017 Aug 17. doi: 10.1093/aje/kwx277. [Epub ahead of print
Research Paper of the Month: Aug. 5, 2017
Both chronic and acute ozone exposure during pregnancy increase the risk of still birth, as much as 39% even at levels below the EPA’s standards. Even the ozone levels in the week prior to delivery increase the risk. About 8,000 still births a year occur nationally due to ozone. Extrapolating from that research to Utah indicates about 100 still births a year occur in Utah due to our ozone, and that doesn’t count the risk of PM2.5.
Mendola P, Ha S, Pollack AZ, Zhu Y, Seeni I, Kim SS, Sherman S, Liu D. Chronic and Acute Ozone Exposure in the Week Prior to Delivery Is Associated with the Risk of Stillbirth.Int J Environ Res Public Health. 2017 Jul 6;14(7). pii: E731. doi: 10.3390/ijerph14070731.
Even air pollution levels slightly above background levels are associated withe increased rates of hospitalization for all causes, and for respiratory and heart problems in particular. Like other studies on mortality, the rate of increase per unit of exposure, was even greater at PM 2.5 levels below 8 ug/m3. The current annual EPA standard is 12. Background levels of PM2.5 are about 5 ug/m3.
Makar M, Antonelli J, Di Q, Cutler D, Schwartz J, Dominici F. Estimating the Causal Effect of Low Levels of Fine Particulate Matter on Hospitalization. Epidemiology. 2017 Sep;28(5):627-634. doi: 10.1097/EDE.0000000000000690.
Ozone is associated with increased rates of hospitalizations for heart attacks.
Chiu HF, Weng YH, Chiu YW, Yang CY. Short-Term Effects of Ozone Air Pollution on Hospital Admissions for Myocardial Infarction: A Time-Stratified Case-Crossover Study in Taipei. J Toxicol Environ Health A. 2017 Jun 9:1-7. doi: 10.1080/15287394.2017.1321092. [Epub ahead of print]
Air pollution exposure of a pregnant mother increases the likelihood of obesity later on in childhood.
Mao G, et al. Individual and Joint Effects of Early-Life Ambient PM2.5 Exposure and Maternal Prepregnancy Obesity on Childhood Overweight or Obesity. Environ Health Perspect; DOI:10.1289/EHP261
More evidence that air pollution increases the risk of intrauterine growth retardation, small for gestational weight babies, and premature births.
Basu R, et al. Association between PM2.5 and PM2.5 Constituents and Preterm Delivery in California, 2000-2006.
Paediatr Perinat Epidemiol. 2017 Jul 21. doi: 10.1111/ppe.12380. [Epub ahead of print]
Clemens T, Turner S, Dibben C. Maternal exposure to ambient air pollution and fetal growth in North-East Scotland: A population-based study using routine ultrasound scans. Environ Int. 2017 Jul 25;107:216-226. doi: 10.1016/j.envint.2017.07.018. [Epub ahead of print]
Liu C, et al. Different exposure levels of fine particulate matter and preterm birth: a meta-analysis based on cohort studies. Environ Sci Pollut Res Int. 2017 Jun 15. doi: 10.1007/s11356-017-9363-0. [Epub ahead of print]
Several recent studies strengthening the connection between air pollution and cancer, especially breast cancer.
Sifaki-Pistolla D, Lionis C, Koinis F, Georgoulias V, Tzanakis N; On behalf of the Cancer Registry of Crete (CRC). Lung cancer and annual mean exposure to outdoor air pollution in Crete, Greece. Eur J Cancer Prev. 2017 Jul 25. doi: 10.1097/CEJ.0000000000000407. [Epub ahead of print]
White AJ, et al. Indoor Wood-Burning Stove and Fireplace Use and Breast Cancer in a Prospective Cohort Study. Environ Health Perspect. 2017 Jul 18;125(7):077011. doi: 10.1289/EHP827.
Large C, Wei Y. Geographic variations in female breast cancer incidence in relation to ambient air emissions of polycyclic aromatic hydrocarbons. Environ Sci Pollut Res Int. 2017 Jun 14. doi: 10.1007/s11356-017-9395-5. [Epub ahead of print]
Goldberg MS, et al. The association between the incidence of postmenopausal breast cancer and concentrations at street-level of nitrogen dioxide and ultrafine particles. Environ Res. 2017 Jun 5;158:7-15. doi: 10.1016/j.envres.2017.05.038. [Epub ahead of print]
Air pollution reduces survival after the diagnosis of liver cancer
Deng H, et al. Particulate matter air pollution and liver cancer survival. Int J Cancer. 2017 Jun 7. doi: 10.1002/ijc.30779. [Epub ahead of print]
More evidence that air pollution is a risk factor for inflammatory bowel disease.
van der Sloot KWJ, Amini M, Peters V, Dijkstra G, Alizadeh BZ. Inflammatory Bowel Diseases: Review of Known Environmental Protective and Risk Factors Involved. Inflamm Bowel Dis. 2017 Aug 2. doi: 10.1097/MIB.0000000000001217. [Epub ahead of print]
More evidence that even short term air pollution decreases lung function in otherwise healthy adults
Panis L, Provost EB, Cox B, Louwies T, Laeremans M, Standaert A, Dons E, Holmstock L, Nawrot T, De Boever P. Short-term air pollution exposure decreases lung function: a repeated measures study in healthy adults. Environ Health. 2017 Jun 14;16(1):60. doi: 10.1186/s12940-017-0271-z. PMID: 28615020 [PubMed – in process]

Research Paper of the Month: July 10, 2017
This is a landmark study on air pollution and mortality, involving 61 million people from throughout the country. It is published in the most prestigious journal in the world, the New England Journal of Medicine. It significantly strengthens the association between premature death and PM2.5 and ozone. The key findings were that levels of both pollutants, well below the EPA’s standards are still strongly associated with mortality. Specifically, for every 10 ug/m3 of chronic PM2.5 exposure mortality in 7.3%, or .73% for every 1 ug/m3. For ozone, for every 10 ppb, the mortality increased 1.1%. However, at lower concentrations, that association was even stronger. For those people exposed to levels of PM2.5 below 12 ug/m3 (the current EPA annual standard), and below 50 ppb ozone (the current EPA standard is 70 ppb), the risk of death increased to 1.36% for every 1 ug/m3 for PM2.5, and continued at the same rate for ozone, i.e. 1% for every 10 ppb.
This is the strongest research statement yet to establish that: 1. There is no safe level of air pollution. 2. Current EPA standards are inadequate and out of step with the science. 3. The health hazard per unit off exposure is actually greater at the lowest doses. That means public policy needs to address the problem even for those cities that have relatively clean air. 4. The current administration’s attempt to delay or role back standards will do even more harm than what has been previously calculated.
Di Q, et al. Air Pollution and Mortality in the Medicare Population. New England Journal of Medicine, 2017; 376 (26): 2513 DOI: 10.1056/NEJMoa1702747
The subjects in this study below were children, teenagers, and young adults in Mexico City where the particulate pollution is still quite high, despite many public policy changes to address it. This is the second study to show that these tiny pollution nanoparticles from fossil fuel combustion end up inside our brains. Once there they can cause brain damage, disrupting cellular and intracellular architecture. This undoubtedly contributes to the many clinical studies that show impaired brain function, loss of memory, loss of intellectual abilities, behavior problems, and more degenerative brain diseases in people exposed to more air pollution.
We should be just as concerned about the air our children breathe as we are about lead in the water they drink.
González-Maciel A, Reynoso-Robles R, Torres-Jardón R, Mukherjee PS, Calderón-Garcidueñas L. Combustion-Derived Nanoparticles in Key Brain Target Cells and Organelles in Young Urbanites: Culprit Hidden in Plain Sight in Alzheimer’s Disease Development. J Alzheimers Dis. 2017 Jun 3. doi: 10.3233/JAD-170012. [Epub ahead of print]
This study shows that heart function is impaired with air pollution.
Yang WY, et al. Left ventricular function in relation to chronic residential air pollution in a general population. Eur J Prev Cardiol. 2017 Jan 1:2047487317715109. doi: 10.1177/2047487317715109. [Epub ahead of print]
Good review on the broad based health consequences of ozone. Think of it as slightly less toxic than particulate pollution.
Nuvolone D, Petri D, Voller F. The effects of ozone on human health. Environ Sci Pollut Res Int. 2017 May 25. doi: 10.1007/s11356-017-9239-3. [Epub ahead of print]
Numerous studies are showing a strong connection between pollution and type II diabetes. This study of newborns showed an increase in insulin levels, measured from cord blood, with more particulate pollution exposure. Specifically, for every 2.4 ug/m3 increase in PM2.5, insulin levels increased 13%. This suggests that pollution in utero can set the stage for type II diabetes later in life.
Madhloum N, et al. Cord plasma insulin and in utero exposure to ambient air pollution. Environ Int. 2017 May 22. pii: S0160-4120(16)30886-8. doi: 10.1016/j.envint.2017.05.012. [Epub ahead of print]
Air pollution can adversely affect heart rhythm.
Carll AP, et al. Inhaled ambient-level traffic-derived particulates decrease cardiac vagal influence and baroreflexes and increase arrhythmia in a rat model of metabolic syndrome. Part Fibre Toxicol. 2017 May 25;14(1):16. doi: 10.1186/s12989-017-0196-2.
Air pollution found to reduce survival after diagnosis of liver cancer
Deng H, et al. Particulate matter air pollution and liver cancer survival. Int J Cancer. 2017 Jun 7. doi: 10.1002/ijc.30779. [Epub ahead of print]
Two more studies showing a relationship between air pollution and breast cancer.
Goldberg MS, et al. The association between the incidence of postmenopausal breast cancer and concentrations at street-level of nitrogen dioxide and ultrafine particles. Environ Res. 2017 Jun 5;158:7-15. doi: 10.1016/j.envres.2017.05.038. [Epub ahead of print]
Large C, Wei Y. Geographic variations in female breast cancer incidence in relation to ambient air emissions of polycyclic aromatic hydrocarbons. Environ Sci Pollut Res Int. 2017 Jun 14. doi: 10.1007/s11356-017-9395-5. [Epub ahead of print]
Ozone is associated with increased rates of hospitalizations for heart attacks.
Chiu HF, Weng YH, Chiu YW, Yang CY. Short-Term Effects of Ozone Air Pollution on Hospital Admissions for Myocardial Infarction: A Time-Stratified Case-Crossover Study in Taipei. J Toxicol Environ Health A. 2017 Jun 9:1-7. doi: 10.1080/15287394.2017.1321092. [Epub ahead of print]
Yet another study showing increased incidence of premature birth with air pollution. The evidence is now overwhelming.
Liu C, et al. Different exposure levels of fine particulate matter and preterm birth: a meta-analysis based on cohort studies. Environ Sci Pollut Res Int. 2017 Jun 15. doi: 10.1007/s11356-017-9363-0. [Epub ahead of print]
Short term air pollution decreases lung function in healthy adults.
Panis L, Provost EB, Cox B, Louwies T, Laeremans M, Standaert A, Dons E, Holmstock L, Nawrot T, De Boever P. Short-term air pollution exposure decreases lung function: a repeated measures study in healthy adults. Environ Health. 2017 Jun 14;16(1):60. doi: 10.1186/s12940-017-0271-z.
Research Paper of the Month: May 27, 2017
This paper gives us new insight into how particulate pollution causes vascular dysfunction, leading to such things heart attacks and strokes. Inhaled nanoparticles were found to accumulate in the lining of blood vessels at sites of existing inflammation and atherosclerosis, aggravating that disease process. The particles appeared in the blood and urine of human subjects within as little as 15 minutes, and were still present three months later.
Miller MR, et al. Inhaled Nanoparticles Accumulate at Sites of Vascular Disease. ACS Nano. 2017 Apr 26. doi: 10.1021/acsnano.6b08551. [Epub ahead of print]
Telomeres are repeating sequences of DNA at the ends of chromosomes that keep the chromosomes from unraveling. Every time the cell divides it loses some telomere length. Telomere length is closely associated with longevity. Previous studies have shown air pollution is associated with shorter placental and fetal telomere length. This study shows that in children and adolescents, air pollution exposure is associated with reduced telomere length, and that means reduced life expectancy.
Lee E, et al. Traffic-Related Air Pollution and Telomere Length in Children and Adolescents Living in Fresno, CA. Journal of Occupational and Environmental Medicine, 2017; 59 (5): 446 DOI: 10.1097/JOM.0000000000000996
As the connection between air pollution and neurodegenerative diseases steadily grows, this is one we didn’t anticipate–air pollution aggravating symptoms of Parkinson’s disease.
Lee H, Myung W, Kim DK, Kim SE, Kim CT, Kim H. Short-term air pollution exposure aggravates Parkinson’s disease in a population-based cohort. Sci Rep. 2017 Mar 16;7:44741. doi: 10.1038/srep44741.
Another study showing that air pollution impairs the vascular architecture of the placenta.
Hettfleisch, K, et al. Short-Term Exposure to Urban Air Pollution and Influences on Placental Vascularization Indexes. Environ Health Perspect; DOI:10.1289/EHP300
Evidence of air pollution’s adverse effect on pregnancy is now overwhelming. In this study particulate pollution was associated with a decrease in fetal thyroid hormone (TSH) and decreased.
Janssen BG, et al. Fetal Thyroid Function, Birth Weight, and in Utero Exposure to Fine Particle Air Pollution: A Birth Cohort Study. Environ Health Perspect; DOI:10.1289/EHP508
Another study showing the connection between air pollution and another pregnancy complication–gestational hypertension.
Zhu Y, et al. Ambient air pollution and risk of gestational hypertension. Am J Epidemiol. 2017 May 4. doi: 10.1093/aje/kwx097. [Epub ahead of print]
Two more studies showing air pollution damages DNA by altering “epigenetics,” the chemical bath that chromosomes sit in.
Lai CH, et al. Exposure to fine particulate matter causes oxidative and methylated DNA damage in young adults: A longitudinal study. Sci Total Environ. 2017 Apr 23;598:289-296. doi: 10.1016/j.scitotenv.2017.04.079. [Epub ahead of print]
Ding R, et al. Dose- and time- effect responses of DNA methylation and histone H3K9 acetylation changes induced by traffic-related air pollution. Sci Rep. 2017 Mar 3;7:43737. doi: 10.1038/srep43737.
Another study showing air pollution impairs our mental health, i.e. is associated with higher rates of anxiety and depression.
Pun VC, et al. Association of Ambient Air Pollution with Depressive and Anxiety Symptoms in Older Adults: Results from the NSHAP Study. Environ Health Perspect; DOI:10.1289/EHP494
Research Paper of the Month: March 7, 2017
Air pollution accelerates brain aging, increases the deposition of amyloid beta particles in the brain, and can almost double the risk of Alzheimer’s in elderly women. Put another way, air pollution appears to be responsible for 20% of Alzheimer’s. A critical Alzheimer risk gene, magnifies the risk further, especially in women, and interacts with air pollution to accelerate brain aging.
Cacciottolo M, et al. Particulate air pollutants, APOE alleles and their contributions to cognitive impairment in older women and to amyloidogenesis in experimental models. Translational Psychiatry (2017) 7, e1022; doi:10.1038/tp.2016.280 Published online 31 January 2017
Research Paper of the Month: Feb. 27, 2017
This study suggests that the real culprit in particulate air pollution’s adverse effect on pregnancy outcomes is PAHs which are often attached to air pollution particles, rather than the particles themselves. More evidence that not all air pollution is created equal, and we should be paying much more attention to those sources that create high levels of PAH pollution–wood smoke, and industrial pollution.
Jedrychowski WA, Majewska R, Spengler JD, Camann D, Roen EL, Perera FP. Prenatal exposure to fine particles and polycyclic aromatic hydrocarbons and birth outcomes: a two-pollutant approach. Int Arch Occup Environ Health. 2017 Feb 7. doi: 10.1007/s00420-016-1192-9. [Epub ahead of print]
The most toxic type of particulate pollution is the ultrafine category, i.e. less than 0.1 micron is size. Ultrafine pollution exposure is associated with accelerated atherosclerosis and increased rates of inflammatory bowel disease. This study reveals a likely mechanism. Ultrafines can be inhaled or ingested. This study shows that ingested ultrafine pollution altered the microbial make up of the bowel, and increased atherogenic lipid metabolites.
Li R, et al. Ambient Ultrafine Particle Ingestion Alters Gut Microbiota in Association with Increased Atherogenic Lipid Metabolites. Sci Rep. 2017 Feb 17;7:42906. doi: 10.1038/srep42906.
Outdoor air pollution has been linked to 2.7 million preterm births per year, 18% of all pre-term births.
Christopher S. Malley, Johan C.I. Kuylenstierna, Harry W. Vallack, Daven K. Henze, Hannah Blencowe, Mike R. Ashmore. Preterm birth associated with maternal fine particulate matter exposure: A global, regional and national assessment. Environment International, 2017; DOI: 10.1016/j.envint.2017.01.023
The closer you live to a major traffic corridor, the greater your chance of developing dementia. More evidence of the neurotoxicity of air pollution.
Chen H, et al. Living near major roads and the incidence of dementia, Parkinson’s disease, and multiple sclerosis: a population-based cohort study. Published: 04 January 2017 DOI: http://dx.doi.org/10.1016/S0140-6736(16)32399-6
Another cancer associated with air pollution—liver cancer.
Pedersen M, et al. Ambient air pollution and primary liver cancer incidence in four European cohorts within the ESCAPE project. Environ Res. 2017 Jan 17;154:226-233. doi: 10.1016/j.envres.2017.01.006. [Epub ahead of print]
Research Paper of the Month: Dec. 30, 2016
The 9/11 dust cloud from the collapse of the Twin Towers in 2001, was shown to be associated with significantly higher rates of premature birth and low birth wt in the babies of pregnant women in Manhattan, nearest the site. The study’s authors stated, “the impacts are especially pronounced for fetuses exposed in the first trimester, and for male fetuses. We estimate that in this group, exposure to the dust cloud more than doubled the probability of premature delivery and had similarly large effects on the probability of low birth weight.” This is more evidence that even short term air pollution exposure can affect the developing fetus, and therefore life long health.
Currie J, et al. The 9/11 Dust Cloud and Pregnancy Outcomes: A Reconsideration
The Journal of Human Resources 51(4):805-831, DOI: 10.3368/jhr.51.4.0714-6533R
More research confirming the connection between air pollution and poor birth outcomes.
Balsa UI, et al. Exposures to Particulate Matter from the Eruptions of the Puyehue Volcano and Birth Outcomes in Montevideo. Environ Health Perspect; DOI:10.1289/EHP235
Exposure to NOx pollution had a significant association with the incidence of a serious pregnancy complication, placental abruption.
Michikawa T, et al. Air Pollutant Exposure within a Few Days of Delivery and Placental Abruption in Japan. Epidemiology. 2016 Dec 1. [Epub ahead of print]
Here is another study showing that air pollution during pregnancy precipitates the chemical markers of inflammation, a prelude to chronic disease vulnerability later in life for those babies.
Martens DS, et al. Neonatal Cord Blood Oxylipins and Exposure to Particulate Matter in the Early-Life Environment: An ENVIRONAGE Birth Cohort Study. Environ Health Perspect. 2016 Nov 4. [Epub ahead of print]
Changes in mitochondrial DNA (mtDNA) can serve as a marker of cumulative oxidative stress. Increased PM2.5 during the third trimester of pregnancy was associated with decreased mtDNA content suggesting heightened sensitivity to this kind biological damage in a fetus.
Rosa MJ, et al. Identifying sensitive windows for prenatal particulate air pollution exposure and mitochondrial DNA content in cord blood. Environ Int. 2016 Nov 11. pii: S0160-4120(16)30741-3. doi: 10.1016/j.envint.2016.11.007. [Epub ahead of print]
UPHE is adamantly opposed to the proposed project to dam the Bear River, reducing the flow to the Great Salt Lake, shrinking the lake, exposing thousands more acres of dry beach, and increasing the severity of dust storms. This study shows that dust storms in North America, like other forms of air pollution, increase mortality within a matter of days.
Crooks JL, et al. The Association between Dust Storms and Daily Non-Accidental Mortality in the United States, 1993–2005. Environ Health Perspect; DOI:10.1289/EHP216
Numerous studies solidify the connection between air pollution and diabetes and impaired glucose metabolism.
Peng C, et al. Particulate Air Pollution and Fasting Blood Glucose in Nondiabetic Individuals: Associations and Epigenetic Mediation in the Normative Aging Study, 2000–2011. Environ Health Perspect; DOI:10.1289/EHP183
Lu MC, et al. Association of temporal distribution of fine particulate matter with glucose homeostasis during pregnancy in women of Chiayi City, Taiwan. Environ Res. 2016 Oct 13;152:81-87. doi: 10.1016/j.envres.2016.09.023. [Epub ahead of print
Toledo-Corral CM, et al. Effects of air pollution exposure on glucose metabolism in Los Angeles minority children. Pediatr Obes. 2016 Dec 6. doi: 10.1111/ijpo.12188. [Epub ahead of print]
Wallwork RS, Colicino E, Zhong J, Kloog I, Coull BA, Vokonas P, Schwartz JD, Baccarelli AA. Ambient Fine Particulate Matter, Outdoor Temperature, and Risk of Metabolic Syndrome. Am J Epidemiol. 2016 Dec 7. [Epub ahead of print]
Ozone was associated with increased rates of hospitalization for dementia in a population in Spain.
Linares C, et al. Short-term association between environmental factors and hospital admissions due to dementia in Madrid. Environ Res. 2016 Oct 27;152:214-220. doi: 10.1016/j.envres.2016.10.020. [Epub ahead of print]
Air pollution’s association with cognitive decline is now well established. This study shows that among older people who also experience socioeconomic stress and disadvantage, that association is even stronger.
Ailshire J, Karraker A, Clarke P. Neighborhood social stressors, fine particulate matter air pollution, and cognitive function among older U.S. adults. Soc Sci Med. 2016 Nov 14;172:56-63. doi: 10.1016/j.socscimed.2016.11.019. [Epub ahead of print]
More evidence that PM 2.5 air pollution is associated with systemic autoimmune rheumatic diseases (SARDs), as well as an increased relative risk for juvenile idiopathic arthritis
Sun G, et al. Association between Air Pollution and the Development of Rheumatic Disease: A Systematic Review. Int J Rheumatol. 2016;2016:5356307. Epub 2016 Oct 25.
This study shows that ultra fine particulate pollution can affect development of the fetal brain by changing the expression of neuroprotective genes on nerve cells.
Solaimani P, Saffari A, Sioutas C, Bondy SC, Campbell A. Exposure to ambient ultrafine particulate matter alters the expression of genes in primary human neurons. Neurotoxicology. 2016 Nov 13. pii: S0161-813X(16)30225-X. doi: 10.1016/j.neuro.2016.11.001. [Epub ahead of print]
More research showing the connection between environmental factors, air pollution in particular, and autism. Autism genes are affected by environmental pollutants.
Morales-Suárez-Varela M, et al. Systematic review of the association between particulate matter exposure and autism spectrum disorders. Environ Res. 2016 Dec 13;153:150-160. doi: 10.1016/j.envres.2016.11.022. [Epub ahead of print]
.
Carter CJ, et al. Autism genes are selectively targeted by environmental pollutants including pesticides, heavy metals, bisphenol A, phthalates and many others in food, cosmetics or household products. Neurochem Int. 2016 Oct 27. pii: S0197-0186(16)30197-8. doi: 10.1016/j.neuint.2016.10.011. [Epub ahead of print]
Children exposed to more traffic pollution short term, score worse on tests of ability to pay attention.
Sunyer J, et al. Traffic-related air pollution and attention in primary school children: short-term association. Epidemiology. 2016 Nov 29. [Epub ahead of print]
Some of the first research showing that air pollution reduces kidney function, even at levels significantly below the national EPA standards.
Raaschou-Nielsen O, et al. Outdoor air pollution and risk for kidney parenchyma cancer in 14 European cohorts. Int J Cancer. 2016 Dec 22. doi: 10.1002/ijc.30587. [Epub ahead of print]
This study shows that for the signature outcome of air pollution exposure, a heart attack, the event is likely to be more immediate in older age groups, and more delayed in younger patients. Nonetheless, younger patients are still sensitive to the cardiovascular effects of air pollution.
Collart P, et al. Short-term effects of air pollution on hospitalization for acute myocardial infarction: age effect on lag pattern. Int J Environ Health Res. 2017 Feb;27(1):68-81. doi: 10.1080/09603123.2016.1268678.
Another study showing that exposure to particulate matter is associated with the thickness of atherosclerosis in the body’s arteries.
Aguilera I, et al. Particulate Matter and Subclinical Atherosclerosis: Associations between Different Particle Sizes and Sources with Carotid Intima-Media Thickness in the SAPALDIA Study. Environ Health Perspect; DOI:10.1289/EHP161
This is intuitively obvious, but this study shows higher rates of exacerbations of COPD with more air pollution.
Li J, et al. Major air pollutants and risk of COPD exacerbations: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2016 Dec 12;11:3079-3091. doi: 10.2147/COPD.S122282. eCollection 2016.
Research Paper of the Month: Oct. 30, 2016
Air pollution has been classified as a “Class I carcinogen” by the World Health Organization. There has been a steady increase in the incidence of Acute Myeloid Leukemia (AML) over the past several decades, and other research implicates air pollution as a trigger for leukemia. This study showed that compared to healthy children, those who had AML had significantly higher levels of “particulate matter derived nanoparticles” aggregated with blood components. This demonstrates a plausible mechanism by which air pollution could trigger AML.
Visani G, et al. Environmental nanoparticles are significantly over-expressed in acute myeloid leukemia. Leuk Res. 2016 Nov;50:50-56.
For every 10 ug/m3 of PM2.5, the risk of intrauterine inflammation (IUI) increased 240%. IUI contributes to, or is a mechanism for, multiple types of pregnancy complications.
Nachman R, et al. Intrauterine Inflammation and Maternal Exposure to Ambient PM2.5 during Preconception and Specific Periods of Pregnancy: The Boston Birth Cohort. Environ Health Perspect; DOI:10.1289/EHP243
This study shows that a 2.1 ug/m3 increase in chronic PM2.5 exposure was associated with a decrease in kidney function equivalent to what would be expected from 2 yrs of aging. Bear in mind that the Wasatch Front averages a PM2.5 of about 10. So that would be a decrease in kidney function equivalent to ten years of aging.
Mehta A, et al. Long-Term Exposure to Ambient Fine Particulate Matter and Renal Function in Older Men: The Veterans Administration Normative Aging StudyEnviron Health Perspect. 2016 Sep; 124(9): 1353–1360.
Even one to two day episodes of air pollution may be enough to trigger premature births.
Li S, et al. Acute Impact of Hourly Ambient Air Pollution on Preterm Birth. Environ Health Perspect; DOI:10.1289/EHP200
This is a review article highlighting the evidence that air pollution exposure during pregnancy and even preconception can affect the fetal development of organs like the lungs.
Veras MM, et al. Before the first breath: prenatal exposures to air pollution and lung development. Cell Tissue Res. 2016 Oct 10. [Epub ahead of print]
More evidence that episodic air pollution, typical of Utah’s inversions, provokes damage to the lining of blood vessels, which can contribute to acceleration of age related vascular disease, and ultimately strokes, heart attacks, sudden death, and poor pregnancy outcomes. The subjects studied were young healthy adults.
Pope CA, Bhatnagar A, McCracken J, Abplanalp WT, Conklin DJ, O’Toole TE. Exposure to Fine Particulate Air Pollution Is Associated with Endothelial Injury and Systemic Inflammation. Circ Res. 2016 Oct 25. pii: CIRCRESAHA.116.309279.
Research Paper of the Month: Sept. 10, 2016
This study documents that toxic, nano-sized particles called “magnetites” found in air pollution end up in our brains. People with higher concentrations of the metallic nanoparticles are known to be at higher risk for Alzheimer’s, and the kind of brain damage these “magnetites” can cause are consistent with the disease.
At 150 nanometers or less in diameter, these particles, including iron oxide, platinum, nickel, and cobalt, whose origin can be industrial, vehicle or other sources of pollution, are small enough to be inhaled through the nose and enter the brain through the olfactory nerve system. The researchers found millions of these particles per gram of brain tissue after studying numerous autopsies. The lead study author said these results are “dreadfully shocking”.
Maher, B, et al. Magnetite pollution nanoparticles in the human brain. PNAS 2016 ; published ahead of print September 6, 2016, doi:10.1073/pnas.1605941113
More evidence that particulate air pollution harms the brain, in this case, decreases cognition in people 50-80 yrs old.
Tzivian L, et al. Long-Term Air Pollution and Traffic Noise Exposures and Mild Cognitive Impairment in Older Adults: A Cross-Sectional Analysis of the Heinz Nixdorf Recall Study. Environ Health Perspect; DOI:10.1289/ehp.1509824
This meta-analysis demonstrated an association between autism NOx and particulate pollution.
Flores-Pajot MC, Ofner M, Do MT, Lavigne E, Villeneuve PJ. Childhood autism spectrum disorders and exposure to nitrogen dioxide, and particulate matter air pollution: A review and meta-analysis. Environ Res. 2016 Aug 25. pii: S0013-9351(16)30317-6. doi: 10.1016/j.envres.2016.07.030. [Epub ahead of print]
More evidence that air pollution increases the risk for insulin resistance and type II diabetes.
Wolf K, Popp A, Schneider A, Breitner S, Hampel R, Rathmann W, Herder C, Roden M, Koenig W, Meisinger C, Peters A; Association Between Long-Term Exposure to Air Pollution and Biomarkers Related to Insulin Resistance, Subclinical Inflammation and Adipokines. Diabetes. 2016 Sep 7. pii: db151567. [Epub ahead of print]
Research Paper of the Month: July 30, 2016
This study showed that the Great London Smog event of 1952, was still impacting people’s health 60 years later. Those who were infants or babies in utero when they were exposed to the event (which only lasted 5 days), showed higher rates of respiratory disease measured several decades later.
Bharadwaj P, et al. Early Life Exposure to the Great Smog of 1952 and the Development of Asthma. Am J Respir Crit Care Med. First published online 08 Jul 2016 as DOI: 10.1164/rccm.201603-0451OC
We have know for several years that even low levels of particulate pollution (PM2.5) are associated with increased rates of daily death. Here is more evidence.
Schwartz J. et al. Estimating Causal Effects of Local Air Pollution on Daily Deaths: Effect of Low Levels. Environ Health Perspect; DOI:10.1289/EHP232
It is well established that air pollution increases human mortality. Here is an interesting study that shows air pollution increases mortality in animals, in this case dairy cows.
Cox B, Gasparrini A, Catry B, Fierens F, Vangronsveld J, Nawrot TS. Ambient Air Pollution-Related Mortality in Dairy Cattle: Does It Corroborate Human Findings? Epidemiology. 2016 Jul 27. [Epub ahead of print]
Air pollution accelerates the aging process, at least in part by shortening the length of telomeres. Life expectancy is proportional to telomere length, and the initial length of telomeres at birth is largely the result of environmental factors. Telomeres can be considered the cellular memories of exposure to oxidative stress and inflammation throughout a life time.
Martens DS, Nawrot TS. Air Pollution Stress and the Aging Phenotype: The Telomere Connection. Curr Environ Health Rep. 2016 Jun 29. [Epub ahead of print]
Air pollution is associated with a loss of the sense of smell (which incidentally is one of the first signs of Alzheimer’s).
Ajmani GS, et al. Effects of Ambient Air Pollution Exposure on Olfaction: A Review. Environ Health Perspect. 2016 Jun 10. [Epub ahead of print]
Mounting evidence on the connection between type II diabetes and air pollution.
Eze IC, et al. Air pollution and diabetes association: Modification by type 2 diabetes genetic risk score. Environ Int. 2016 Jun 6;94:263-271. doi: 10.1016/j.envint.2016.04.032. [Epub ahead of print]
Goettems-Fiorin PB, et al. Fine particulate matter potentiates type 2 diabetes development in high-fat diet-treated mice: stress response and extracellular to intracellular HSP70 ratio analysis. J Physiol Biochem. 2016 Jun 29. [Epub ahead of print]
Communities with higher air pollution see more prescription use of medications for psychiatric disorders.
Oudin, A., Bråbäck, L., Oudin Åström, D., Strömgren, M., Forsberg, B.: Association between neighbourhood air pollution concentrations and dispensed medication for psychiatric disorders in a large longitudinal cohort of Swedish children and adolescents. BMJ Open 2016;6:e010004 doi:10.1136/bmjopen-2015-010004
More research showing the effect of air pollution on pregnancy and fetal development
Impaired fetal growth, fetal loss, and neonatal deaths were significantly associated with heavy metals exposure during pregnancy.
Rahman A, Kumarathasan P, Gomes J. Infant and mother related outcomes from exposure to metals with endocrine disrupting properties during pregnancy. Sci Total Environ. 2016 Jul 1. pii: S0048-9697(16)31309-2. doi: 10.1016/j.scitotenv.2016.06.134. [Epub ahead of print]
This study demonstrated that the number of blood vessels in the placenta is decreased in the first trimester among women exposed to more NO2.
Hettfleisch K, et al. Short-Term Exposure to Urban Air Pollution and Influences on Placental Vascularization Indexes. Environ Health Perspect. 2016 Jul 6. [Epub ahead of print]
Particulate pollution is associated with higher rates of heart birth defects
Liu CB, et al. Effects of Prenatal PM10 Exposure on Fetal Cardiovascular Malformations in Fuzhou, China: A Retrospective Case-Control Study. Environ Health Perspect. 2016 Jul 6. [Epub ahead of print]
Vanadium is a heavy metal that has been recently recognized as a significant toxin, and is emitted as a byproduct of fossil fuel combustion, especially common in refinery emissions. The more vanadium in a mother’s body, the higher the rate of low birthweight
Jiang M, et al. A nested case-control study of prenatal vanadium exposure and low birthweight. Hum Reprod. 2016 Jul 4. pii: dew176. [Epub ahead of print]
More evidence that toxic compounds in air pollution, from traffic and industrial sources, can cause cancer, in this case brain cancer in children with in utero, or infancy exposure.
von Ehrenstein O, et al. In Utero and Early-Life Exposure to Ambient Air Toxics and Childhood Brain Tumors: A Population-Based Case–Control Study in California, USA Environ Health Perspect; DOI:10.1289/ehp.1408582
Kawasaki Disease is an inflammation of the blood vessels that afflicted infants an young children. This study showed a statistical association between KD and ozone exposure. Air pollution certainly causes inflammation, so this is not a surprise.
Jung CR, et al. Ambient Air Pollutant Exposures and Hospitalization for Kawasaki Disease in Taiwan: A Case-Crossover Study (2000-2010) Environ Health Perspect; DOI:10.1289/EHP137
Research Paper of the Month: May 28, 2106
This is probably the best study to date showing that air pollution does indeed increase risk for still births. This meta-analysis showed a 2% increase for every 4 ug/m3 PM2.5. During a bad winter inversion and the height of the Uinta Basin drilling activity, at the one poorly placed monitor in Vernal, there was often PM2.5 of over 60. If that monitor had been placed in downtown Vernal, it would very likely have been much worse. Winter inversions in the Salt Lake Valley can reach PM2.5 levels of over 90. NOx, SO2, CO, and ozone were also shown to significantly correlate with still births. Vernal has had the unique distinction of simultaneously high ozone, and high PM2.5.
Siddika N, Balogun HA, Amegah AK, Jaakkola JJ. Prenatal ambient air pollution exposure and the risk of stillbirth: systematic review and meta-analysis of the empirical evidence. Occup Environ Med. 2016 May 24. pii: oemed-2015-103086. doi: 10.1136/oemed-2015-103086. [Epub ahead of print] Review.
The study below showed that the multi-faceted operations of the Canadian Tar Sands are a major source of air pollution in North America. The authors state this has implications for other sources of “heavy oil” extraction. That would include the heavy black wax crude in the Uinta Basin. These two studies certainly reinforce our concern about air pollution as the most likely explanation for the spike in infant deaths in Vernal.
Leggy J, et al. Oil sands operations as a large source of secondary organic aerosols Nature (2016) doi:10.1038/nature17646
This is a landmark study showing chronic PM 2.5 levels of as little as 5 ug/m3 correlate with a 20% increase in development of coronary artery calcification over ten years. The EPA’s annual standard is 12.5 ug. So based on the metric from this study, what the EPA considers “safe” or acceptable, will increase the “hardening” of your arteries over 70 yrs, by 360%. Doesn’t sound very safe does it?
Kaufman, J, et al. Association between air pollution and coronary artery calcification within six metropolitan areas in the USA (the Multi-Ethnic Study of Atherosclerosis and Air Pollution): a longitudinal cohort study. DOI: http://dx.doi.org/10.1016/S0140-6736(16)00378-0
The risk of a ischemic stroke with air pollution is well established. This study shows that particulate pollution and ozone are significantly correlated with hemorrhagic stroke as well.
Han M, et al. Association between hemorrhagic stroke occurrence and meteorological factors and pollutants. BMC Neurol. 2016 May 4;16(1):59. doi: 10.1186/s12883-016-0579-2.
More evidence on the association between air pollution and type II diabetes. This study is from China, where the air pollution is particularly severe.
Liu C, et al. Associations between long-term exposure to ambient particulate air pollution and type 2 diabetes prevalence, blood glucose and glycosylated hemoglobin levels in China. Environ Int. 2016 May 2;92-93:416-421. doi: 10.1016/j.envint.2016.03.028. [Epub ahead of print]
Research Paper of the Month: May 1, 2016
Following almost 67,000 people, researchers found there is a strong correlation between chronic exposure to particulate pollution, and death due to all types of cancer. In particular for every 10 ug/m3 of PM2.5 (which is about the annual average for the Wasatch Front), there was an overall increase of 22% in death from cancer, and even higher rates for lung and digestive system cancers, and an extraordinary increase of 80% in death rates for breast cancer, the most common cancer in women. Any of your loved ones have breast cancer? This should make the issue of air quality very personal to everyone.
Wong CM, et al. Cancer Mortality Risks from Long-term Exposure to Ambient Fine Particle. Cancer Epidemiol Biomarkers Prev; Published OnlineFirst April 29, 2016; doi 10.1158/1055-9965.EPI-15-0626
This will likely be considered a landmark study. It shows that even air quality we label
“good,” or “green”, i.e. PM2.5 of about 10 ug/m3, doubles the incidence of “intrauterine inflammation” which is a strong predisposition for premature birth. Furthermore, it shows that level of pollution even in the first three months prior to conception, increases the risk of intrauterine inflammation 52%.
Nachman RM, et al. Intrauterine Inflammation and Maternal Exposure to Ambient PM2.5 during Preconception and Specific Periods of Pregnancy: The Boston Birth Cohort. Environ Health Perspect. 2016 Apr 27. [Epub ahead of print]
UPHE has been beating the drum on all the medical research showing how toxic air pollution is to the brain. Here is yet another study showing impairment of cognitive abilities and memory in eight year old school children.
Basagaña X, et al. Neurodevelopmental Deceleration by Urban Fine Particles from Different Emission Sources: A Longitudinal Observational Study. Environ Health Perspect. 2016 Apr 29;124(5). [Epub ahead of print]
This study shows that hourly levels of air pollution at the time labor begins, show a significant correlation with rates of premature birth.
Li S, Guo Y, Williams G. Acute Impact of Hourly Ambient Air Pollution on Preterm Birth. Environ Health Perspect. 2016 Apr 29. [Epub ahead of print]
Another study showing air pollution is associated with depression–in this case PM2.5 of 10 ug/m3 associated with about a 50% increase.
Kim KN, et al. Long-Term Fine Particulate Matter Exposure and Major Depressive Disorder in a Community-Based Urban Cohort. Environ Health Perspect. 2016 Apr 29. [Epub ahead of print]
More evidence that short-term exposure to PM2.5 promotes type II diabetes, by inducing vascular insulin resistance and inflammation triggered by a mechanism involving inflammation in the lungs.
Haberzettl P, O’Toole TE, Bhatnagar A, Conklin DJ. Exposure to Fine Particulate Air Pollution Causes Vascular Insulin Resistance by Inducing Pulmonary Oxidative Stress. Environ Health Perspect. 2016 Apr 29. [Epub ahead of print]
Another study showing air pollution changes the placental epigenetic profile, putting a newborn at risk for adverse health outcomes later in life.
Tsamou M, et al. Air pollution-induced placental epigenetic alterations in early life: a candidate miRNA approach. Epigenetics. 2016 Apr 22:0. [Epub ahead of print]
Exposure to traffic related pollution at birth was associated with a 500% increased risk for a certain type of childhood leukemia (AML).
Janitza AE, et al. Traffic-related air pollution and childhood acute leukemia in Oklahoma. Environmental Research. Volume 148, July 2016, Pages 102–111
Children exposed to more traffic related air pollution at home, have lower grade point averages, even when other known confounding variables are factored in.
Clark-Reyna SE, et al. Residential exposure to air toxics is linked to lower grade point averages among school children in El Paso, Texas, USA. Popul Environ. 2016 Mar;37(3):319-340. Epub 2015 Jul 17.
Prenatal exposure to NOx is associated with increased risk for childhood obesity
Lavigne E, et al. Air Pollution Exposure During Pregnancy and Fetal Markers of Metabolic Function: The MIREC Study. Am J Epidemiol. 2016 Mar 29. pii: kwv256. [Epub ahead of print]
Measuring PAH (polycyclic aromatic hydrocarbons)/DNA adducts from umbilical cord blood (as an indication of air pollution exposure), there was a significant correlation between prenatal air pollution exposure and anxiety, depression, aggressive behavior, and attention problems in children up to 11 years old.
Margolis AE, et al. Longitudinal effects of prenatal exposure to air pollutants on self-regulatory capacities and social competence. J Child Psychol Psychiatry. 2016 Mar 17. doi: 10.1111/jcpp.12548. [Epub ahead of print]
This study found a 24% increase in type II diabetes per increase in long term exposure to PM2.5 of 3.1 ug/m3 (less than a third of annual average on the Wasatch Front).
Hansen AB, et al. Long-term exposure to fine particulate matter and incidence of diabetes in the Danish Nurse Cohort. Environ Int. 2016 Mar 15;91:243-250. doi: 10.1016/j.envint.2016.02.036. [Epub ahead of print]
Among elderly men, air pollution aggravates cardiovascular risk factors, i.e. increased blood pressure, decreased heart rate variability, worse cholesterol profile, and inflammatory biomarkers. Those effects were generally more pronounced in men who are already at increased risk of cardiovascular disease
Bind MA, et al. Quantile Regression Analysis of the Distributional Effects of Air Pollution on Blood Pressure, Heart Rate Variability, Blood Lipids, and Biomarkers of Inflammation in Elderly American Men: The Normative Aging Study. Environ Health Perspect. 2016 Mar 11. [Epub ahead of print]
Research Paper of the Month: March 12, 2016
Acrolein, one of the most toxic components in wood smoke, causes deterioration of heart muscle function after 3 hr exposure. Deterioration persisted at least as long as 24 hrs. This study done in mice.
Thompson LC, et al. Acrolein Inhalation Alters Myocardial Synchrony and Performance at and Below Exposure Concentrations that Cause Ventilatory Responses. Cardiovasc Toxicol. 2016 Feb 19. [Epub ahead of print]
High levels of traffic air pollution are associated with significantly higher rates of brain cancer.
Poulsen AH, et al. Air pollution from traffic and risk for brain tumors: a nationwide study in Denmark. Cancer Causes Control. 2016 Feb 18. [Epub ahead of print]
More evidence of air pollution’s effect on pregnancy. Primary and secondary particulate matter, NOx, and ozone were all associated with higher incidences of pre-term births.
Laurent O, et al. A Statewide Nested Case-Control Study of Preterm Birth and Air Pollution by Source and Composition: California, 2001-2008. Environ Health Perspect. 2016 Feb 19. [Epub ahead of print]
Habitual incense burning in the home is associated with decreased birth weight and small head circumference in term births. Boys are affected more than girls.
Chen LY, et al. Incense Burning during Pregnancy and Birth Weight and Head Circumference among Term Births: The Taiwan Birth Cohort Study. Environ Health Perspect. 2016 Mar 11. [Epub ahead of print]
PM2.5, and NOx are associated with higher rates of Low Birth Weight Syndrome.
Coker E, et al. Multi-pollutant exposure profiles associated with term low birth weight in Los Angeles County. Environ Int. 2016 Feb 15;91:1-13. doi: 10.1016/j.envint.2016.02.011. [Epub ahead of print]
Research Paper of the Month: March 1, 2016
The evidence for air pollution’s neurotoxicity continues to mount. For every 3 ug/m3 increase in NO2, considered a marker of traffic pollution, rates of Parkinson’s Disease increased 9%. Wasatch Front averages around 25 ug/m3. This study suggests that Wasatch Front pollution is associated with an increase in Parkinson’s of 72%.
Ritz B, et al. Traffic-Related Air Pollution and Parkinson’s Disease in Denmark: A Case–Control Study. Environ Health Perspect; DOI:10.1289/ehp.1409313
Long term exposure to traffic pollution strongly associated with Alzheimer’s and vascular caused dementia.
Oudin, A, et al. Traffic-Related Air Pollution and Dementia Incidence in Northern Sweden: A Longitudinal Study. Environ Health Perspect; DOI:10.1289/ehp.1408322
Air pollution over Manhattan, 1970s.
Research Paper of the Month: Feb. 17, 2016
The evidence on how air pollution damages the brain continues to mount. This study followed almost 100,000 people’s chronic air pollution exposure, and found an extraordinary 211% risk of Alzheimer’s per increase of 10.91 ppb in O3, a 138% risk of increase of AD per increase of 4.34 μg/m3 in PM2.5. Ozone can reach 70-80 ppb in the summer, and PM2.5 70-90 ug/m3 in the winter.
Jung CR, Lin YT, Hwang BF. Ozone, particulate matter, and newly diagnosed Alzheimer’s disease: a population-based cohort study in Taiwan. J Alzheimers Dis. 2015;44(2):573-84. doi: 10.3233/JAD-140855.
Research Paper of the Month: Feb. 12, 2016
This fascinating study demonstrates that the increased mortality affect of air pollution persists for decades. The air pollution you breathed in the 1970s is still increasing your mortality risk.
Hansell A, et al. Historic air pollution exposure and long-term mortality risks in England and Wales: prospective longitudinal cohort study. Thorax 2015;0:1–9. doi:10.1136/thoraxjnl-2015-207111
The body of research revealing the neurotoxicity of air pollution, especially polycyclic aromatic hydrocarbons (PAHs) continues to grow. This study in people over 60 yrs. old, showed this correlation between metabolites of PAHs measured in urine and cognitive testing: a 1% increase in PAHs resulted in approximately a 1.8% poorer performance.
Best EA, Juarez-Colunga E, James K, LeBlanc WG, Serdar B (2016) Biomarkers of Exposure to Polycyclic Aromatic Hydrocarbons and Cognitive Function among Elderly in the United States (National Health and Nutrition Examination Survey: 2001-2002). PLoS ONE 11(2): e0147632. doi:10.1371/journal.pone.0147632
There is a growing body of research showing a significant connection between air pollution and Type II diabetes, i.e. decreased glucose tolerance, and insulin sensitivity. This study showed short term air pollution has these effects as well as increasing bad cholesterol (LDL) , and decreasing the good cholesterol (HDL).
Chen Z, et al. Ambient Air Pollutants Have Adverse Effects on Insulin and Glucose Homeostasis in Mexican Americans. Diabetes Care. 2016 Feb 11. pii: dc151795. [Epub ahead of print]
Another meta-analysis showing the connection between air pollution and multiple types of adverse pregnancy outcomes.
Lamichhane DK, Leem JH, Lee JY1, Kim HC. A meta-analysis of exposure to particulate matter and adverse birth outcomes. Environ Health Toxicol. 2015 Nov 3;30:e2015011. doi: 10.5620/eht.e2015011. eCollection 2015.
Research Paper of the Month: Jan. 17, 2016
A 32 study meta-analysis showing significant association between PM2.5 exposure during the second and third trimesters and lower overall birth weights, and higher rates of babies who qualify as having Low Birth Weight Syndrome. Heavy metals and PAHs likely increase the toxicity of PM2.5 in causing this outcome. The authors state, “These robust results further reveal the toxic effect of PM2.5 exposure during pregnancy on fetal growth. Air pollution is ubiquitous. All pregnant women are exposed to it at some level, and immature fetuses are more susceptible.”
Sun X, Luo X, Zhao C, Zhang B, Tao J, Yang Z, Ma W, Liu T. The associations between birth weight and exposure to fine particulate matter (PM<sub>2.5</sub>) and its chemical constituents during pregnancy: A meta-analysis. Environ Pollut. 2015 Dec 28;211:38-47. doi: 10.1016/j.envpol.2015.12.022. [Epub ahead of print]
More evidence that PM2.5 pollution is associated with increased risk for pre-term birth.
DeFranco E, et al. Exposure to airborne particulate matter during pregnancy is associated with preterm birth: a population-based cohort study. Environ Health. 2016 Jan 15;15(1):6. doi: 10.1186/s12940-016-0094-3.
Even more evidence that air pollution reduces the birth weight of infants. Babies born in Beijing, China during 2008 when significant reductions in pollution were achieved for the Olympics, babies born were larger than those born in the year before and the year after.
Rich D, et al. Differences in Birth Weight Associated with the 2008 Beijing Olympic Air Pollution Reduction: Results from a Natural Experiment. Environ Health Perspect; DOI:10.1289/ehp.1408795
Pregnant mothers exposed to more wood smoke, give birth to children that demonstrate worse neurologic scores including visuo-spatial integration, short-term memory, long-term memory, and fine motor skills when tested at ages 6-7.
Cooper L, Eskenazi B, Romero C, Balmes J, Smith KR. Neurodevelopmental performance among school age children in rural Guatemala is associated with prenatal and postnatal exposure to carbon monoxide, a marker for exposure to woodsmoke. Neurotoxicology. 2012 Mar;33(2):246-54. doi: 10.1016/j.neuro.2011.09.004. Epub 2011 Sep 24.
Air pollution associated with higher rates of heart birth defects.
Girguisa M, et al. Maternal exposure to traffic-related air pollution and birth defects in Massachusetts. Environmental Research. Volume 146, April 2016, Pages 1–9
Numerous studies have shown that air pollution is significantly correlated with rates of Type II diabetes. This study shows the possible biologic mechanism–increased levels of circulating stress hormones and lipid metabolites with even brief exposure to high levels of ozone.
Miller D, et al. Ozone Exposure Increases Circulating Stress Hormones and Lipid Metabolites in Humans. Am J Respir Crit Care Med. 2016 Jan 8. [Epub ahead of print]
Air pollution exposure during fetal development and infancy can have life long consequences. This study showed decreased lung function measured at age 16 for those adolescents that were exposed to more air pollution during the first year of life. Additional pollution exposure after that, caused further reductions in lung function.
Schultz E, et al. “Early-Life Exposure to Traffic-related Air Pollution and Lung Function in Adolescence”, American Journal of Respiratory and Critical Care Medicine, Vol. 193, No. 2 (2016), pp. 171-177.
Chronic exposure to PM2.5 is associated with loss of brain white matter in elderly women. For every 3.49 ug/m3 PM2.5 annual average, the loss of white matter was about what would be seen from 1-2 years of aging. With Salt Lake City averaging about 10 ug/m3, that means there is an acceleration of brain aging of 3-6 yrs.
Chen JC, et al. Ambient Air Pollution and Neurotoxicity on Brain Structure: Evidence From Women’s Health Initiative Memory Study. ANN NEUROL 2015;78:466–476
Research Paper of the Month: Dec. 12, 2015
This MIT study is from 2013, and we don’t know how we missed this at the time, but it certainly ramps up the relationship between pollution and mortality. Epidemiologic evidence indicates that annually, 210,000 people in the US die prematurely due to particulate pollution and ozone. And the average premature death represents a loss of life of ten years!
PM2.5 generated from coal and diesel combustion are much more potent triggers of cardiovascular disease than PM2.5 from other sources.
Thurston GD, Burnett RT, Turner MC, Shi Y, Krewski D, Lall R, Ito K, Jerrett M, Gapstur SM, Diver WR, Pope CA 3rd. Ischemic Heart Disease Mortality and Long-Term Exposure to Source-Related Components of U.S. Fine Particle Air Pollution. Environ Health Perspect. 2015 Dec 2. [Epub ahead of print]
More exposure to particulate pollution is associated with higher blood levels of triglycerides and total cholesterol.
Shanley RP, Hayes RB, Cromar KR, Ito K, Gordon T, Ahn J. “Particulate Air Pollution and Clinical Cardiovascular Disease Risk Factors”. Epidemiology. 2015 Nov 24. [Epub ahead of print]
More evidence of the neurotoxicity of air pollution
Costa LG, et al. NEUROTOXICITY OF TRAFFIC-RELATED AIR POLLUTION. Neurotoxicology. 2015 Nov 20. pii: S0161-813X(15)30024-3. doi: 10.1016/j.neuro.2015.11.008. [Epub ahead of print]
Particulate pollution associated with higher rates of hospital admissions for multiple sclerosis.
Laura A,, et al. Effects of particulate matter exposure on multiple sclerosis hospital admission in Lombardy region, Italy. Environ Res. 2015 Nov 25;145:68-73. doi: 10.1016/j.envres.2015.11.017. [Epub ahead of print]
Decreased lung function in children postnatally exposed to pesticides.
Raanan R, Balmes JR, Harley KG, Gunier RB, Magzamen S, Bradman A, Eskenazi B. Decreased lung function in 7-year-old children with early-life organophosphate exposure. Thorax. 2015 Dec 3. pii: thoraxjnl-2014-206622. doi: 10.1136/thoraxjnl-2014-206622. [Epub ahead of print]
Elderly people exposed to more air pollution have impaired heart electrical activity (prolonged QT interval).
Mordukhovich I, Kloog I, Coull B, Koutrakis P, Vokonas P, Schwartz J. Association between Particulate Air Pollution and QT Interval Duration in an Elderly Cohort. Epidemiology. 2015 Nov 24. [Epub ahead of print]
Research Paper of the Month: Nov. 21, 2015
More evidence that air pollution causes poor pregnancy outcomes, especially pre-term births.
Sun X, et al. The association between fine particulate matter exposure during pregnancy and preterm birth: a meta-analysis. BMC Pregnancy Childbirth. 2015 Nov 18;15(1):300.
.
Zhu X, et al. Maternal exposure to fine particulate matter (PM2.5) and pregnancy outcomes: a meta-analysis. Environ Sci Pollut Res Int. 2015 Mar;22(5):3383-96. doi: 10.1007/s11356-014-3458-7. Epub 2014 Aug 28.
PM2.5 is associated with increased risk for liver cancer.
Pan W, et al. Fine Particle Pollution, Alanine Transaminase, and Liver Cancer: A Taiwanese Prospective Cohort Study (REVEAL-HBV). J Natl Cancer Inst. 2015 Nov 11;108(3). pii: djv341. doi: 10.1093/jnci/djv341. Print 2015 Mar.
Hazardous air pollutant exposure during prenatal life and early infancy are strongly associated with increased rates of certain types of childhood brain tumors.
von Ehrenstein O, et al. In Utero and Early-Life Exposure to Ambient Air Toxics and Childhood Brain Tumors: A Population-Based Case–Control Study in California, USA. Environ Health Perspect; DOI:10.1289/ehp.1408582
More evidence that pre-natal pollution harms brain function in children. In this case NOx exposure was calculated at birth, verbal IQ tests were done at age seven.
Porta D, Narduzzi S, Badaloni C, Bucci S, Cesaroni G, Colelli V, Davoli M, Sunyer J, Zirro E, Schwartz J, Forastiere F. Air pollution and cognitive development at age seven in a prospective Italian birth cohort. Epidemiology. 2015 Sep 30. [Epub ahead of print]
The bulk of the evidence suggests that people benefit from exercise, even during pollution situations. But what is the threshold at which someone does themselves more harm than good is not known. Aerobic exercise augments the overall inhaled air pollution dose, potentiates the diffusion of pollutants into circulating blood, augments oxidative stress and inflammation, raises blood pressure, impairs vascular function, and unfavorably affect autonomic balance.
Giorgini P, Rubenfire M, Bard RL, Jackson EA, Ferri C, Brook RD. Air Pollution and Exercise: A REVIEW OF THE CARDIOVASCULAR IMPLICATIONS FOR HEALTH CARE PROFESSIONALS. J Cardiopulm Rehabil Prev. 2015 Sep 16. [Epub ahead of print]
New methodology that solidifies the increase in mortality due to air pollution.
Schwartz J, Austin E, Bind MA, Zanobetti A, Koutrakis P. Estimating Causal Associations of Fine Particles With Daily Deaths in Boston. Am J Epidemiol. 2015 Sep 6. pii: kwv101. [Epub ahead of print]
More research strengthening the connection between air pollution and Alzheimer’s and dementia. Rates increased about 40% for the most exposed group, compared to the least.
Oudin A, Forsberg B, Nordin Adolfsson A, Lind N, Modig L, Nordin M, Nordin S, Adolfsson R, Nilsson LG. Traffic-Related Air Pollution and Dementia Incidence in Northern Sweden: A Longitudinal Study. Environ Health Perspect. 2015 Jul 31. [Epub ahead of print]
Research Paper of the Month: Oct. 15, 2015
Pregnant mothers who live closest to fracking sites were 40% more likely to give birth prematurely than those who live farthest away. Premature birth predisposes a baby to a lifelong increase in vulnerability to a wide variety of poor health outcomes.
Casey JA, Savitz DA, Rasmussen SG, Ogburn EL, Pollak J, Mercer DG, Schwartz BS. Unconventional Natural Gas Development and Birth Outcomes in Pennsylvania, USA. Epidemiology. 2015 Sep 30. [Epub ahead of print]
Pregnant mothers more exposed to neurotoxins in air pollution, in this case styrene and chromium are more likely to give birth to children who are later diagnosed with autism. It is unclear, however, whether these chemicals are risk factors themselves or if they are just a reflection of the effect of a much larger mixture of toxic compounds.
Talbott EO, et al. Air toxics and the risk of autism spectrum disorder: the results of a population based case-control study in southwestern Pennsylvania. Environ Health. 2015 Oct 6;14:80. doi: 10.1186/s12940-015-0064-1.
Research Paper of the Month: May 21, 2015
Another study showing significantly increased risk for Autism Spectrum Disorder with prenatal, and post natal (up to two years after birth) exposure to PM2.5.
Talbott E, et al. Fine particulate matter and the risk of autism spectrum disorder. Environmental Research. Volume 140, July 2015, Pages 414–420
Research Paper of the Month: May 15, 2015
This paper followed 10 million people, and measured the time to first admission for any of three neurodegenerative diseases–dementia, Alzheimer’s, or Parkinson’s. They found an 8-15% increase in diagnosis of these disorders per 1 ug/m3 increase in long PM2.5 exposure. That’s a remarkably strong correlation.
Kioumourtzoglou MA, Schwartz JD, Weisskopf MG, Melly SJ, Wang Y, Dominici F, Zanobetti A. Long-term PM2.5 Exposure and Neurological Hospital Admissions in the Northeastern United States. Environ Health Perspect. 2015 May 15. [Epub ahead of print]
Interesting paper that showed decreased birth weight and smaller head circumference in babies born to white, British mothers exposed to more PM2.5, but not in Pakistani mothers. In contrast, more PM2.5 exposure increased adiposity of newborns in Pakistani mothers, but not in white British mothers. Not sure what to make of those findings.
Schembari A, de Hoogh K, Pedersen M, Dadvand P, Martinez D, Hoek G, Petherick ES, Wright J, Nieuwenhuijsen MJ. Ambient Air Pollution and Newborn Size and Adiposity at Birth: Differences by Maternal Ethnicity (the Born in Bradford Study Cohort). Environ Health Perspect. 2015 May 15. [Epub ahead of print]
Research Paper of the Month: May 2, 2015
In Beijing China, for about one month prior to the 2008 Olympics, many of their coal fired power plants were shut down, and traffic was forcibly reduced about 50%, all in an effort to reduce pollution. In a study of 84,000 births, mothers in their 8th month of pregnancy in 2008, compared to 2007 and 2009, gave birth to babies about 1% larger. This then is yet another study showing that air pollution reduces birth weight. 1% doesn’t sound like much per baby, but it becomes a very large public health issue when thousands of babies are affected that way. Reduced birth weight is associated with an increased risk of numerous lifelong chronic diseases and impaired organ function.
Rich D, et al. Differences in Birth Weight Associated with the 2008 Beijing Olympic Air Pollution Reduction: Results from a Natural Experiment. Environ Health Perspect; DOI:10.1289/ehp.1408795
Research Paper of the Month: April 23, 2015
There are now several studies linking air pollution to Type I Diabetes. Two more have been published in the last two weeks.
Bodin J, Stene LC, Nygaard UC. Can Exposure to Environmental Chemicals Increase the Risk of Diabetes Type 1 Development? Biomed Res Int. 2015;2015:208947. Epub 2015 Mar 26.
Malmqvist E. Maternal exposure to air pollution and type 1 diabetes – Accounting for genetic factors. Environ Res. 2015 Apr 13;140:268-274. doi: 10.1016/j.envres.2015.03.024. [Epub ahead of print]
More and more studies are showing how toxic air pollution is to the brain. Previous studies have shown loss of white matter volume in children exposed to air pollution in the womb, and in animals exposed shortly after birth. The study below, examining adults 60 yrs old and older, shows a loss of total brain volume (an indicator of dementia and brain atrophy) with even small increments of PM2.5. For every 2 ug/m3 increase in PM2.5, brain volume decreased 0.32% and the odds of covert brain infarcts (mini-strokes) increased 46%. Given that the EPA has recently lowered the annual PM2.5 standard to 12 ug/m3, that means air quality can meet the national standard, and still be responsible for a 2% decrease in your brain matter, and a 280% increased likelihood of provoking mini-strokes.
Wilker E, et al. Long-Term Exposure to Fine Particulate Matter, Residential Proximity to Major Roads and Measures of Brain Structure. doi: 10.1161/STROKEAHA.114.008348. Published online before print April 23, 2015,
Research Paper of the Month: April 14, 2015
Yet another study showing prenatal air pollution exposure is associated with significantly worse neuropsychological development in children. For every 1 ug/m3 increase in PM2.5, motor scores were decreased 1.14 points, and every 1 ug/m3 increase in NO2 was associated with a 0.29 point decrease in mental scores. The Wasatch Front averages 38-57 ug/m3 for NO2.
Lertxundi A, et al. Exposure to fine particle matter, nitrogen dioxide and benzene during pregnancy and cognitive and psychomotor developments in children at 15months of age. Environ Int. 2015 Apr 10;80:33-40. doi: 10.1016/j.envint.2015.03.007. [Epub ahead of print]
April 5, 2015
Prenatal exposure to pollution increases newborns’ blood pressure.
van Rossem L, et al. Prenatal Air Pollution Exposure and Newborn Blood Pressure. Environ Health Perspect; DOI:10.1289/ehp.1307419
Pregnant mothers exposed to air pollution demonstrate shortened placental telomeres. Placental telomeres correlate with newborn’s telomeres and telomeres are highly predictive of life expectancy. There is wide variability in the length of newborn’s telomeres, and most of that variability is related to environmental exposures. Bottom line–Maternal exposure to air pollution programs her baby to a shorter life span.
Bijnens E, Zeegers MP, Gielen M, Kicinski M, Hageman GJ, Pachen D, Derom C, Vlietinck R, Nawrot TS. Lower placental telomere length may be attributed to maternal residential traffic exposure; a twin study. Environ Int. 2015 Mar 7;79:1-7. doi: 10.1016/j.envint.2015.02.008. [Epub ahead of print]
PAH exposure during pregnancy decreases levels of BDNF (Brain Derived Neurotrophic Factor), critical to brain development, and whose levels correlate inversely with brain dysfunction.
Tang D, Lee J, Muirhead L, Li TY, Qu L, Yu J, et al. 2014. Molecular and neurodevelopmental benefits to children of closure of a coal burning power plant in China. PLoS One 9:e91966.
March 27, 2015
This was a big week in air pollution research.
Prenatal exposure to PAH air pollutants (in high concentrations in refinery emissions, cigarette smoke and wood smoke) damages fetal brain development, shrinking the volume of white matter primarily in the left hemisphere measured in early childhood, resulting in impaired cognition, ADHD and hyperactive behavior.
Peterson B, et al. Effects of Prenatal Exposure to Air Pollutants (Polycyclic Aromatic Hydrocarbons) on the Development of Brain White Matter, Cognition, and Behavior in Later Childhood. JAMA Psychiatry. Published online March 25, 2015.doi:10.1001/jamapsychiatry.2015.57
Large study, examining 350,000 births, at PM2.5 levels of slightly more than 16 ug/m3 in the third trimester, showed 42% increased risk of still births.
DeFranco E, et al. Air Pollution and Stillbirth Risk: Exposure to Airborne Particulate Matter during Pregnancy Is Associated with Fetal Death. PLoS One. 2015 Mar 20;10(3):e0120594. doi: 10.1371/journal.pone.0120594.
Previous studies have shown higher rates of virtually every type of adverse pregnancy outcome with air pollution. This study of 410, 000 pregnant women showed even higher rates of gestational diabetes with air pollution–20% increase for every 5 ug/m3 of PM2.5 and 18% increase for every 5 ppb of ozone.
Hu H, Ha S, Henderson BH, Warner TD, Roth J, Kan H, Xu X. Association of Atmospheric Particulate Matter and Ozone with Gestational Diabetes Mellitus. Environ Health Perspect. 2015 Mar 20. [Epub ahead of print]
March 24, 2015
Large meta-analysis of 94 studies showed even short term spikes in ozone, carbon monoxide, SO2, NOx, and PM2.5 are associated with significant increases in rates of strokes. The greatest association was for the same day of exposure, although PM2.5 showed a lingering affect.
Shah A, et al. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ 2015;350:h1295
March 5, 2105
From the world’s most prestigious medical journal, the New England Journal of Medicine, a landmark study showing improved air quality pays off with improved lung function and actual growth of lung capacity in children. This not only improves cardiovascular capability, but is a key factor in avoiding adult onset of lung and heart disease and increasing life expectancy, which is highly correlated with lung function.
Gauderman WJ, et al. Association of Improved Air Quality with Lung Development in Children. N Engl J Med 2015; 372:905-913March 5, 2015DOI: 10.1056/NEJMoa1414123
March 5, 2015. Another study showing kids exposed to more traffic pollution demonstrate intellectual impairment compared to their non-exposed peers. In this study, similar to other studies, the cognitive loss was over 4%.
Sunnier J, et al. Association between Traffic-Related Air Pollution in Schools and Cognitive Development in Primary School Children: A Prospective Cohort Study. PLOS medicine. Published: March 3, 2015DOI: 10.1371/journal.pmed.1001792
Feb. 28, 2015
Even a modest program of curtailing community wood smoke in the San Joaquin Valley resulted in a significant reduction in PM2.5, about 15%, and a similar reduction in hospitalization for ischemic heart disease. Salt Lake City would undoubtedly have an even greater benefit because the average winter temperature in Salt Lake is about ten degrees colder than the San Joaquin Valley, therefore more wood is being burned.
Yap PS, Garcia C. Effectiveness of Residential Wood-Burning Regulation on Decreasing Particulate Matter Levels and Hospitalizations in the San Joaquin Valley Air Basin. Am J Public Health. 2015 Feb 25:e1-e7. [Epub ahead of print]
Feb. 16, 2015
Another recent study compared daily hospital admissions and death rates related to cardiovascular and pulmonary diseases among two cities in South America where one city’s pollution was predominantly from wood smoke and another was from mobile and typical point sources. Compared to the non-wood burning city, the city with primarily wood smoke experienced an increase of 47% for cardiorespiratory deaths, and an increase of 104% for respiratory hospital admissions for every 10 ug/m3 increase in PM10
Díaz-Robles L, et al. Short Term Health Effects of Particulate Matter: A Comparison between Wood Smoke and Multi-Source Polluted Urban Areas in Chile. Aerosol and Air Quality Research, 15: 306–318, doi:10.4209/aaqr.2013.01.0316